Loading
Get Prior Authorization Request Form Fax To Wellcare
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Request Form FAX To WellCare online
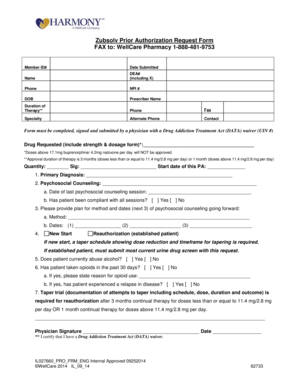
The Prior Authorization Request Form FAX To WellCare is a crucial document for users seeking authorization for specific medications. This guide provides clear and step-by-step instructions to help you complete the form accurately and efficiently.
Follow the steps to fill out the form correctly.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin by filling out the member ID number at the top of the form, ensuring you provide accurate and current information.
- Input the date you are submitting the request, as well as the name of the prescribing physician.
- Enter the prescriber’s DEA number, which includes the X designation if applicable. This is necessary for compliance with treatment regulations.
- Provide the prescriber’s phone number, NPI number, date of birth, and contact details to ensure you can be reached for any follow-up.
- List the drug requested, ensuring to include the strength and dosage form, as requests exceeding specified dosages will not be approved.
- Indicate the quantity requested and provide the starting date for this prior authorization.
- Complete the primary diagnosis section with appropriate details regarding the condition being treated.
- Document the psychosocial counseling provided, including the date of the last session and whether the patient complied.
- Outline the future plan for psychosocial counseling, including methods and specific dates for upcoming sessions.
- Mark whether the request is for a new start or reauthorization, ensuring to follow any required documentation guidelines for each.
- Answer questions regarding the patient’s alcohol abuse history and past opioid use, providing specific details where required.
- Finally, the prescriber must sign the form and date it, certifying they possess the necessary waiver under the Drug Addiction Treatment Act.
- Review all information for accuracy and completeness before saving changes, downloading, printing, or sharing the completed form.
Take action now and complete your Prior Authorization Request Form online today!
Redeterminations (Part D Appeals) If we deny your request for a coverage determination (exception), or a payment for a drug, you, your doctor, or your representative may ask us for a redetermination. You have 60 days from the date of our coverage denial letter to request a redetermination.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


