Loading
Get Prior Authorization Request - Hormonal Therapy Prior Authorization Request - Hormonal
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Request - Hormonal Therapy Prior Authorization Request - Hormonal online
Completing the Prior Authorization Request for hormonal therapy is a crucial step to ensure the prescribed medication is covered by the patient's benefit plan. This guide provides clear and step-by-step instructions to help users accurately fill out the form online.
Follow the steps to complete the Prior Authorization Request effectively.
- Click ‘Get Form’ button to obtain the form and open it in your selected editor.
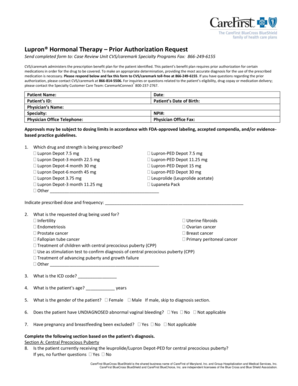
- Enter the date and patient details, including their date of birth, name, and identification number accurately.
- Fill in the physician's information, such as their name, specialty, office telephone number, NPI number, and fax number.
- Select the drug and strength being prescribed from the provided options and indicate the prescribed dose and frequency.
- Specify the reason for requesting the drug by selecting from the listed options and providing any additional details as needed.
- Input the patient's ICD code and age in the designated fields.
- Indicate the gender of the patient and answer any relevant questions pertaining to their medical history and diagnosis.
- Complete sections A through H based on the patient's specific diagnosis, responding truthfully to questions and providing supporting documentation where necessary.
- Review the information entered to ensure accuracy and completeness before signing the form.
- Once all sections are filled, save your changes, and choose whether to download, print, or share the completed form for submission.
Complete the prior authorization request online for hormonal therapy to ensure timely medication coverage.
As is within a protected drug class, prior authorization will not be required for members who are actively taking this medication. The table below outlines circumstances under which prior authorization is needed and not needed for .
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


