Loading
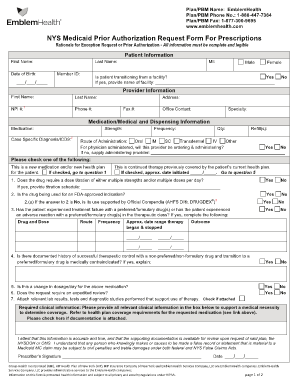
Get Emblem Prior Authorization Request Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Emblem Prior Authorization Request Form online
Completing the Emblem Prior Authorization Request Form online can be a straightforward process when you know the necessary steps. This guide will provide you with clear and detailed instructions for each section of the form to ensure that all required information is accurately submitted.
Follow the steps to efficiently complete the form.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Start by entering the patient's information. Fill in the first name, last name, middle initial, date of birth, and member ID. Ensure that this information is complete and legible.
- Next, provide the provider's information, including their first name, last name, NPI number, address, phone number, fax number, office contact, and specialty.
- In the medication and medical information section, specify the medication name, strength, case-specific diagnosis/ICD-10, frequency of usage, quantity, and the number of refills needed. Select the route of administration as appropriate.
- Indicate whether the medication is a new therapy or a continuation from a previous health plan. Check the applicable box to clarify this status.
- Complete the clinical necessity questions by answering 'Yes' or 'No' to each. Provide any additional details requested based on your responses, especially if the drug requires dose titration or is being used for an FDA-approved indication.
- Attach any relevant lab results or medical documentation that supports the necessity of the requested medication. Ensure all supporting documents are either attached or checked as applicable.
- Finally, review all entered information for accuracy, provide the prescriber’s signature, and date the form. Once you have confirmed that all required fields are complete, save changes, and prepare to submit the document.
Complete your Emblem Prior Authorization Request Form online now to ensure timely processing of your request.
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


