Get Alameda Alliance Medication Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Alameda Alliance Medication Prior Authorization Form online
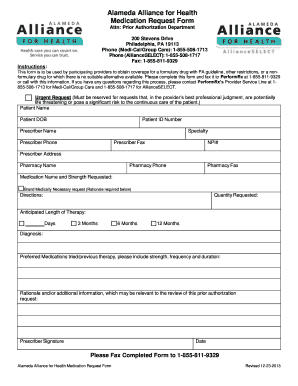
Filling out the Alameda Alliance Medication Prior Authorization Form is an essential step for participating providers seeking coverage for specified medications. This guide provides clear, step-by-step instructions to streamline the process of completing the form online.
Follow the steps to effectively complete the form.
- Press the ‘Get Form’ button to access the medication request form and ensure it opens properly for editing.
- Begin with the patient information section. Fill out the patient's name, date of birth, and patient ID number accurately to ensure proper identification.
- In the prescriber section, provide your name, specialty, phone number, fax number, and NPI number. This information is crucial for any follow-up communication.
- List the pharmacy's name, phone number, and fax number to facilitate the medication order process.
- Specify the medication name and strength requested. If applicable, check the box for 'Brand Medically Necessary request' and provide the rationale if the medication is not a standard formulary option.
- Indicate the directions for medication usage, quantity requested, and the anticipated length of therapy by selecting the appropriate time frame (e.g., Days, 3 Months, 6 Months, or 12 Months).
- Provide the diagnosis related to the medication request to give context for the prior authorization.
- Document any preferred medications that have been tried previously, including strength, frequency, and duration of use. This helps in illustrating the case for the request.
- If necessary, include a rationale and any additional information that may be relevant to the review of your prior authorization request.
- Finally, sign and date the form in the prescriber signature section before submission.
- After completing the form, save your changes, then download, print, or share the form as needed. Fax the completed form to 1-855-811-9329.
Start filling out the Alameda Alliance Medication Prior Authorization Form online today to ensure timely processing of your medication requests.
Use Our Automated Eligibility Verification Line! Our Automated Eligibility Verification Line has been updated to provide better customer service to our providers. Alliance providers can now call 1.510. 747.4505, 24 hours and 7 days a week, to verify patient eligibility.
Fill Alameda Alliance Medication Prior Authorization Form
Complete the attached PA request form. Alameda Alliance for Health. Referral and Prior Authorization (PA) Procedure Codes Utilization Management (UM) Medications. To ensure medication safety to patients through the verification of all medication orders prior to dispensing. POLICY. Use this form to submit prior authorization requests for Physician-Administered Drugs to the Alliance. Fax to the Alliance Pharmacy Department at .
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


