Loading
Get Prior Authorization Form - Magellan Pharmacy Solutions
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form - Magellan Pharmacy Solutions online
This guide provides a comprehensive walkthrough on how to fill out the Prior Authorization Form for Magellan Pharmacy Solutions online. By following these steps, you can ensure that all necessary information is accurately submitted to facilitate the prior authorization process.
Follow the steps to complete the form accurately.
- Click ‘Get Form’ button to obtain the Prior Authorization Form and open it in your selected editor.
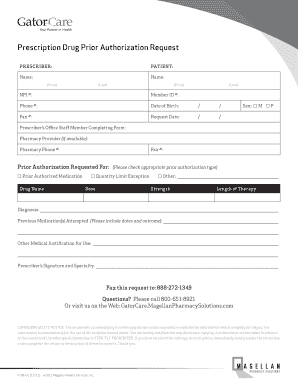
- Fill in the prescriber's information. Enter the prescriber's name, NPI number, and phone number in the designated fields. Make sure that all data is accurate to avoid delays.
- Next, provide detailed patient information including the patient's name, member ID, date of birth, sex, and phone number. Ensure that each field is filled out completely.
- Indicate who from the prescriber's office is completing the form by filling in their name, along with the pharmacy provider details if available, including the pharmacy's phone and fax numbers.
- In the section ‘Prior Authorization Requested For’, select the appropriate authorization type by checking the corresponding box for the medication request, quantity limit exception, or other specifications.
- Input the requested drug's name, dose, strength, and length of therapy in the respective fields to specify the medication required for the patient.
- Provide the diagnosis in detail, as this information supports the request. Be thorough in your explanation to justify the need for the medication.
- List any previous medications that have been attempted, noting the dates and outcomes for each. This history is critical for the prior authorization process.
- Include any additional medical justification for the requested medication in the space provided to strengthen the request.
- Lastly, the prescriber must sign the form, indicating their specialty. After completing the form, review all entries for accuracy.
- Once you have confirmed that all information is correct, you can save changes, download the completed form, and print or share it as required.
Complete your Prior Authorization Form online to facilitate your medication request process.
If your insurance company denies pre-authorization, you can appeal the decision or submit new documentation. By law, the insurance company must tell you why you were denied. Then you can take the necessary steps to get it approved.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


