Get Prior Auth Form (2) - Superior Healthplan
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Auth Form (2) - Superior HealthPlan online
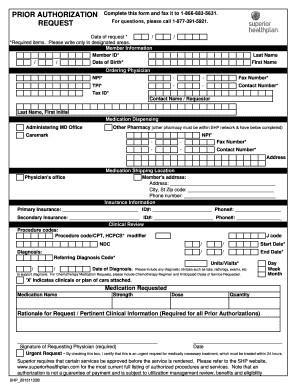
Filling out the Prior Auth Form (2) - Superior HealthPlan online is essential for obtaining necessary authorizations for medical services. This guide will walk you through each section of the form, ensuring you understand the information required for a complete submission.
Follow the steps to fill out the Prior Auth Form accurately.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin by entering the date of your request in the designated field. Ensure that all required items are filled out accurately.
- Fill in the member information, including the member ID, date of birth, last name, and first name.
- Next, provide details for the ordering physician. This includes their NPI, fax number, contact number, TPI, and tax ID. Make sure to include the name of the contact person or requestor in the appropriate fields.
- Complete the medication dispensing section. If applicable, ensure that the pharmacy is within the Superior HealthPlan network and fill out their NPI, fax number, contact number, and address.
- In the insurance information section, provide the primary and secondary insurance details, including insurance names, ID numbers, and phone numbers.
- Move on to the clinical review section. Here, include the procedure codes, diagnosis details, and any related clinicals to support your request.
- Fill out the medication requested section by providing the medication name, strength, dose, and quantity.
- Provide a rationale for the request along with pertinent clinical information. This section is required for all prior authorizations.
- Date and sign the form as the requesting physician. If this request is urgent, check the box to indicate urgency.
- After reviewing the form for completeness, you can save changes, download, print, or share the form as needed.
Take action now by completing the Prior Auth Form (2) - Superior HealthPlan online to ensure timely processing of your request.
To begin the enrollment, visit the TMHP How to Apply for Enrollment page . All providers will use the Provider Enrollment and Management System (PEMS) to complete the enrollment process. Resources for enrollment: TMHP provider enrollment representative at 800-925-9126, Option 3.
Fill Prior Auth Form (2) - Superior HealthPlan
Complete this form and fax it to 1-. Superior Health Plan has partnered with CoverMyMeds to offer electronic prior authorization (ePA) services. Need to perform a pre-auth check? Use the Ambetter from Superior HealthPlan Pre-Auth Tool to approve vision, dental, and behavioral health services. Some medical services require approval from Superior HealthPlan. This is called prior authorization. Please read all instructions below before completing this form. Please send this request to the issuer from whom you are seeking authorization. Effective March 18, 2021, Superior HealthPlan will launch new outpatient fax forms for requesting Prior Authorization (PA) for transplant services.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


