Loading
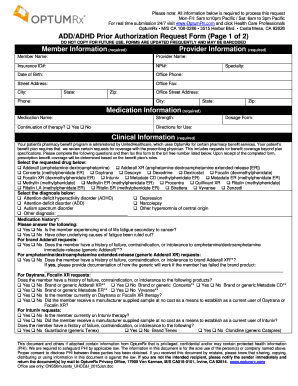
Get Add/adhd Prior Authorization Request Form (page 1 Of ... - Optumrx
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the ADD/ADHD Prior Authorization Request Form (Page 1 Of ... - OptumRx online
Filling out the ADD/ADHD Prior Authorization Request Form is a crucial step in securing necessary medication for individuals diagnosed with ADHD or ADD. This guide provides clear, step-by-step instructions on how to accurately complete the form, ensuring all required information is submitted for timely processing.
Follow the steps to effectively complete the ADD/ADHD Prior Authorization Request Form
- Press the ‘Get Form’ button to access the ADD/ADHD Prior Authorization Request Form for completion.
- In the 'Member Information' section, provide the member's full name, insurance ID number, date of birth, and contact information, including phone number and address.
- Fill in the 'Provider Information' section with the provider's name, NPI number, and contact details including office phone and fax numbers.
- In the 'Medication Information' section, specify the medication name, strength, and whether this is a continuation of therapy. Provide directions for use and dosage form.
- Complete the 'Clinical Information' section by selecting the requested medication and diagnosis from the provided options and answering any related questions, ensuring to document prior medication history as necessary.
- Provide detailed answers to questions related to previous medication failures or contraindications for specified medications if applicable.
- If additional comments or relevant information is available, fill in the provided space in the last section of the form.
- Review all entries to ensure accuracy and completeness before submission.
- After ensuring all information is correctly filled in, choose to save changes, download, print, or share the filled form as required.
Complete your ADD/ADHD Prior Authorization Request Form online for a smoother and more efficient process.
The prior authorization process begins when a service prescribed by a patient's physician is not covered by their health insurance plan. Communication between the physician's office and the insurance company is necessary to handle the prior authorization.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


