Loading
Get Unicare Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Unicare Prior Authorization Form online
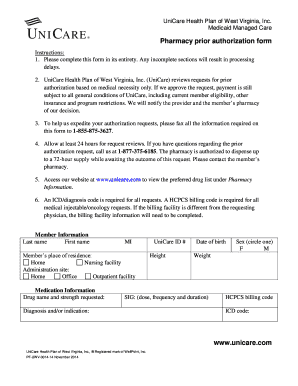
Filling out the Unicare Prior Authorization Form correctly is essential for ensuring that your request for medication is processed efficiently. This guide provides a step-by-step approach to completing the form online, helping users navigate each section with ease.
Follow the steps to complete the online form accurately.
- Press the ‘Get Form’ button to access and open the Unicare Prior Authorization Form in your preferred online document editor.
- Begin by filling out the member information section. Enter the last name, first name, and middle initial of the member. Indicate the member's place of residence by selecting either 'Home' or 'Nursing facility' as applicable.
- In the medication information section, provide the drug name and strength being requested. Also, enter the UniCare ID number, height, date of birth, weight, dosage instructions (SIG), diagnosis or indication for the medication, and the member’s sex.
- If applicable, detail any previous medications the member has tried for their condition, including drug names, strengths, and the date range of use. Otherwise, explain why no alternatives were attempted.
- Discuss any adverse reactions or inadequate responses experienced by the member and provide a brief overview in the allotted space. Mention any pertinent details that may support the request.
- Clearly describe the medical necessity for any non-preferred medications or prescriptions that fall outside FDA labeling guidelines in the provided section.
- List all current medications being taken by the member, including dosage and frequency, as well as any additional relevant information.
- Complete the diagnostic studies and laboratory tests section by listing all tests related to the diagnosis that were performed within the past 30 days, detailing dates and results.
- In the prescriber information section, enter the prescriber's last name, first name, NPI number, DEA/license number, service address, and relevant contact information.
- Fill out the billing facility information, including the facility name, NPI/Tax ID, address, and contact details.
- Provide the pharmacy information by listing the pharmacy name, NPI number, and contact details.
- Confirm the accuracy of the information by signing the form either by the prescriber or an authorized representative. Include the date of signature.
- After completing the form, save your changes. Depending on your needs, you can download, print, or share the completed Unicare Prior Authorization Form.
Complete your Unicare Prior Authorization Form online today to ensure swift processing of your request.
What happens if prior authorization is denied? If your insurance company denies pre-authorization, you can appeal the decision or submit new documentation. By law, the insurance company must tell you why you were denied. Then you can take the necessary steps to get it approved.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


