Loading
Get Prior Authorization Form - Affinity Health Plan - Affinityplan
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form - Affinity Health Plan - Affinityplan online
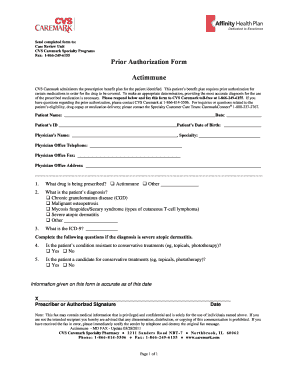
This guide provides a detailed overview of how to fill out the Prior Authorization Form for Affinity Health Plan online. Following these steps can help ensure that the necessary information is accurately submitted for medication coverage.
Follow the steps to complete the form effectively.
- Click ‘Get Form’ button to obtain the Prior Authorization Form and open it in your preferred editor.
- Enter the patient’s name in the designated field, along with their date of birth and ID number. Accurate patient identification is critical for processing the request.
- Provide the physician's name, specialty, office telephone number, fax number, and office address in the respective sections. This information is essential for communication regarding the authorization.
- In the section asking about the prescribed drug, write '' or any other medication being requested. Clearly state the drug to avoid misunderstandings.
- Select the relevant diagnosis for the patient from the listed options, which may include chronic granulomatous disease, malignant osteopetrosis, or severe atopic dermatitis. Choose 'Other' if the diagnosis is not listed and specify.
- Provide the ICD-9 code if available in the specified field to represent the diagnosis accurately. This code is necessary for insurance and billing purposes.
- If the diagnosis is severe atopic dermatitis, answer the follow-up questions regarding the patient's treatment history, indicating whether their condition is resistant or whether they are a candidate for conservative treatments.
- Finally, the prescriber or authorized individual must sign and date the form in the designated area. This signature verifies that the information provided is accurate as of that date.
- Once all sections of the form are filled out, review your entries for accuracy, save any changes made, and prepare to submit the completed form.
- Fax the completed form to CVS Caremark at 1-866-249-6155. Ensure all information is clear to facilitate the processing of the authorization.
Complete your Prior Authorization Form online today to ensure timely medication coverage.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


