Loading
Get Northwood Prior Authorization Request Form For ... - Northwood Inc.
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
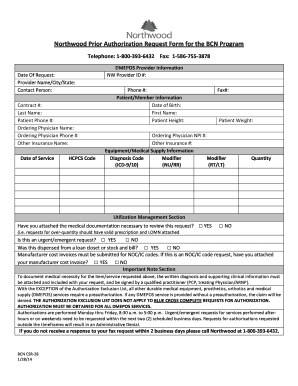
How to fill out the Northwood Prior Authorization Request Form for the BCN Program online
This guide provides users with step-by-step instructions on completing the Northwood Prior Authorization Request Form for the BCN Program. By following these clear and concise directives, you can ensure that your submission process is smooth and accurate.
Follow the steps to complete your form effectively.
- Press the ‘Get Form’ button to obtain the form and open it in the editor for completion.
- Fill in the 'Date of Request' at the top of the form, ensuring the date reflects when you are submitting the request.
- Input the 'Last Name' and 'Patient Phone #' of the individual associated with the request.
- Complete the 'Other Insurance Name' section if applicable, along with the 'Date of Service' to indicate when the service is required.
- Fill in the 'HCPCS Code' and 'DMEPOS Provider Information' sections, including 'NW Provider ID #' and 'Phone #.'
- Provide the 'Patient/Member Information' including 'Date of Birth,' 'First Name,' 'Patient Height,' 'Patient Weight,' and the 'Ordering Physician NPI #.'
- Enter relevant 'Other Insurance #' and the 'Equipment/Medical Supply Information,' detailing 'Diagnosis Code' and 'Modifiers,' as applicable.
- In the 'Quantity' field, specify the necessary amount of equipment or supplies being requested.
- In the 'Utilization Management Section,' indicate if you have attached required medical documentation and whether this is an urgent or emergent request.
- Ensure that any required invoices or medical necessity documentation are completed and attached, particularly for NOC/IC code requests.
- Review the 'Important Note Section' to understand the requirements for authorization and to confirm all necessary information is included.
- After finalizing the form, save your changes and choose to download, print, or share the form as necessary.
Complete your Northwood Prior Authorization Request Form online today for a smooth submission process.
Prior authorization (prior auth, or PA) is a management process used by insurance companies to determine if a prescribed product or service will be covered. This means if the product or service will be paid for in full or in part.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


