Loading
Get Prior Authorization Form - Priority Health
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form - Priority Health online
Filling out the Prior Authorization Form for Priority Health can seem daunting, but this guide will walk you through each step in a clear and supportive manner. By following these instructions, you can ensure that all necessary information is provided accurately and efficiently.
Follow the steps to complete the form successfully
- Find and press the ‘Get Form’ button to access the form and open it in your document editor.
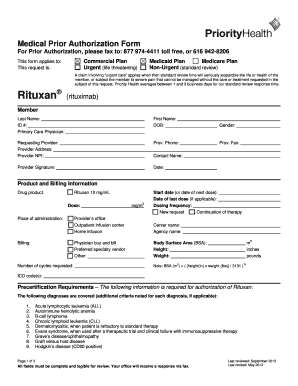
- Begin by entering the member’s last name, first name, date of birth, and ID number in the designated fields. Ensure that this information is accurate as it will be crucial for processing.
- Next, fill in the contact details for the primary care physician, including their name, address, phone number, and fax number. Make sure all fields are legible.
- Proceed to the requesting provider section. Input the requesting provider’s name, address, and their National Provider Identifier (NPI). This information helps identify the provider responsible for this request.
- Fill in the product and billing information, specifying the drug product (e.g., 10 mg/mL), the dosage, and the number of cycles requested. Provide details about the place of administration and the expected start date.
- Make sure to input the patient's body surface area (BSA), height, and weight in the respective fields. Use the formula provided in the form to determine the BSA, ensuring all information is accurate.
- In the precertification requirements section, clearly outline the patient's diagnosis and include any relevant ICD codes. Be precise, as the accuracy of this information is critical for authorization.
- Lastly, review all the entered information for completeness and clarity. Once you are satisfied that all fields are filled out correctly, you can either save your changes, download a copy of the form, print it, or share it as needed.
Start filling out the Prior Authorization Form online today to ensure a smooth process.
Call the phone number on your member ID card or sign in to your health plan account and review your benefits to learn if prior authorization is needed.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


