Loading
Get Specialty Prior Authorization Request Form - Professionals...
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Specialty Prior Authorization Request Form - Professionals online
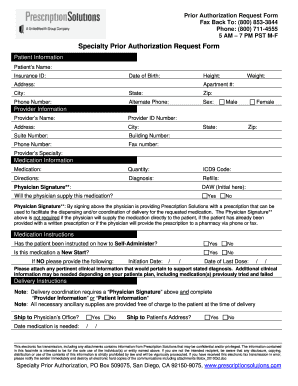
Filling out the Specialty Prior Authorization Request Form online can seem daunting, but a systematic approach can simplify the process. This guide provides clear instructions for each section of the form, ensuring that all necessary information is accurately submitted.
Follow the steps to effectively complete the form.
- Press the ‘Get Form’ button to access the Specialty Prior Authorization Request Form online.
- Begin with the patient information section. Fill in the patient's name, insurance ID, date of birth, height, weight, address, city, state, zip code, primary phone number, alternate phone number, and sex.
- Next, move to the provider information. Enter the provider's name, provider ID number, address, city, suite number, building number, phone number, fax number, state, zip code, and specialty.
- Proceed to the medication information section. Specify the medication name, quantity, ICD9 code, directions, diagnosis, and refills. Sign the physician signature field as necessary.
- In the medication instructions area, indicate whether the patient has been instructed on how to self-administer and if this medication is a new start. If not, provide the initiation date and last dose date.
- Complete the delivery instructions section. Choose whether to ship to the physician's office or the patient's address and specify the date medication is needed.
- Review the form for accuracy. Ensure all necessary fields are completed and that any required clinical information is attached.
- Finally, save any changes you've made to the form. You can then download, print, or share the completed document as needed.
Complete the Specialty Prior Authorization Request Form online today for a streamlined submission process.
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


