Loading
Get Prior Authorization Request Form ... - Optumrx
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Request Form - OptumRx online
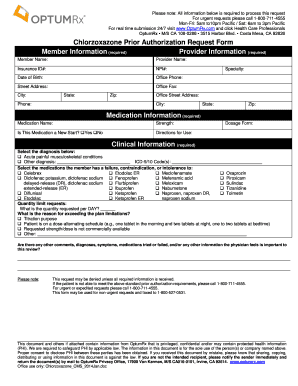
The Prior Authorization Request Form - OptumRx is a critical document for healthcare professionals seeking approval for specific medications. This guide provides clear, step-by-step instructions to help users accurately complete the form online, ensuring all necessary information is submitted for efficient processing.
Follow the steps to fill out the form correctly.
- Begin by selecting the ‘Get Form’ button to access the Prior Authorization Request Form. This action will allow you to open the document in your designated editor for editing.
- Fill in the member information section, which is required. Include the member's name, insurance ID number, date of birth, and mailing address, making sure to provide accurate details to avoid processing delays.
- Complete the provider information section. List the provider's name, NPI number, office phone, fax number, and address. This ensures that the request is associated with the correct healthcare professional.
- In the medication information section, specify the medication's name and strength. Indicate whether this is a new start by selecting 'Yes' or 'No' and provide directions for use and dosage form.
- Select the appropriate diagnosis from the clinical information section. If the condition is not listed, provide a description along with the relevant ICD-9/10 code.
- Document any medications the member has previously tried, specifying any failures, contraindications, or intolerances. This information is crucial for establishing the medical necessity of the requested medication.
- If requesting a quantity limit, detail the quantity requested per day and provide valid reasons for exceeding standard limits.
- Add any additional comments or important details regarding diagnoses, symptoms, or other medications that may be relevant to this request.
- Review all entered information for accuracy. Once complete, save your changes, and choose to download, print, or share the completed form as needed.
Complete your Prior Authorization Request Form online for efficient processing and approval.
Providers can submit their requests to the OptumRx® prior authorization department by completing the applicable form (Part D, UnitedHealthcare or OptumRx) and faxing it to 1-800-527-0531. For urgent requests, call 1-800-711-4555.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


