Loading
Get Prior Authorization Request Form - Geisinger Health Plan
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Request Form - Geisinger Health Plan online
This guide provides clear, step-by-step instructions on how to appropriately fill out the Prior Authorization Request Form for Geisinger Health Plan online. By following these instructions, users can ensure their requests are submitted correctly and efficiently.
Follow the steps to complete the form effectively.
- Click ‘Get Form’ button to acquire the Prior Authorization Request Form and open it in your document editor.
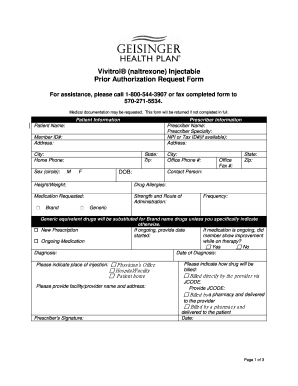
- Begin by filling out the 'Patient Information' section. Include the patient's name, member ID, address, city, home phone number, date of birth, height, weight, and any known drug allergies.
- Proceed to the 'Prescriber Information' section. Enter the prescriber's name, specialty, NPI or Tax ID number, office address, city, state, zip code, and office phone number.
- In the 'Medication Requested' section, specify the medication along with its strength, route of administration, and frequency. Check the box for new prescriptions if applicable.
- If the medication is ongoing, provide the date it was started and indicate whether the member showed improvement while on therapy.
- Complete the 'Diagnosis' section by noting the date of diagnosis and specifying the place of injection, whether at a physician's office, hospital/facility, or patient home.
- Clarify how the drug will be billed by selecting the appropriate option regarding billing directly by the provider or through a pharmacy.
- In the subsequent questions, answer the inquiries regarding the patient's medical history and participation in relevant management programs, ensuring all necessary documentation is enclosed.
- If this is a reauthorization request, provide the requested documentation that supports the request, along with details of the member's current status.
- After completing all fields and ensuring all required sections are filled, save the form. You can then download, print, or share the completed document as needed.
Complete your Prior Authorization Request Form online today to ensure timely processing.
The initial submission of any claim must be received by GHP within 4 months of the date of service for outpatient claims and/or 4 months of the date of discharge for inpatient claims, as applicable.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


