Loading
Get Trillium Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Trillium Prior Authorization Form online
Filling out the Trillium Prior Authorization Form online can streamline the process of obtaining necessary medical authorizations. This guide offers a step-by-step approach to ensure your submission is complete and accurate, thereby increasing the likelihood of approval.
Follow the steps to successfully complete the Trillium Prior Authorization Form
- Press the ‘Get Form’ button to access the form and have it displayed in your online editor.
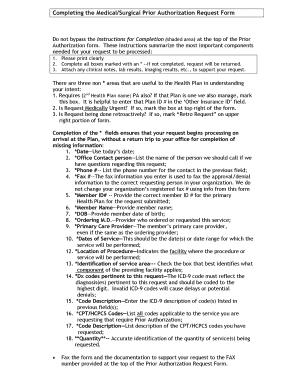
- Read the Instructions for Completion at the top of the form carefully; these highlight critical areas that must be addressed to process your request.
- Print the form clearly to avoid misunderstandings; completeness is key.
- Complete all fields marked with an asterisk (*). If any required fields are left blank, your request will be returned.
- Attach relevant clinical notes, lab results, and imaging results that will support your request.
- In the non-asterisk areas, you may indicate if another health plan requires prior authorization, whether the request is medically urgent, or if it is being submitted retroactively.
- Supply the current date in the *Date field.
- Provide the name of the office contact person in the *Office Contact Person section.
- List the phone number for the contact in the *Phone # field.
- Fill in the *Fax #, ensuring it’s accurate for receiving approval or denial information.
- Enter the *Member ID# for the primary health plan connected to this request.
- Provide the *Member Name of the individual for whom the services are being requested.
- Input the *DOB (date of birth) of the member.
- Specify the *Ordering M.D. — who requested the service.
- List the *Primary Care Provider's name, even if it’s the same as the ordering physician.
- Indicate the *Dates of Service — the specific date or range when services will occur.
- Fill in the *Location of Procedure, detailing where the service will be provided.
- Check the box in the *Identification of Service Area to identify the relevant component of the healthcare facility.
- Provide pertinent *Dx codes relevant to the request, making sure to use the proper ICD-9 format.
- Enter the corresponding *Code Description for the listed diagnostic codes.
- List the necessary *CPT/HCPCS Codes required for prior authorization.
- Describe the *Code Description for each CPT/HCPCS code provided.
- Finally, accurately note the **Quantity of services being requested.
- Fax the completed form along with all supporting documentation to the fax number listed at the top of the Prior Authorization Request Form.
Complete the Trillium Prior Authorization Form online today for an expedited processing experience.
Trillium Community Health Plan payor ID number is 68069.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


