Loading
Get Prior Authorization Form - Swhp
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form - Swhp online
Filling out the Prior Authorization Form - Swhp online can streamline the process of obtaining coverage for necessary medications. This guide provides step-by-step instructions to ensure your submission is complete and accurate.
Follow the steps to efficiently complete the Prior Authorization Form - Swhp online.
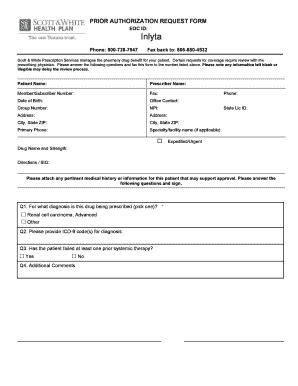
- Press the ‘Get Form’ button to access the Prior Authorization Form - Swhp online and open it in your form editor.
- Begin by entering the patient’s full name in the designated field. This ensures that the request is linked to the correct individual.
- Input the prescriber’s name in the appropriate section to verify who is making the request.
- Fill in the member or subscriber number to associate the request with the correct insurance policy.
- Provide the patient's date of birth to help confirm their identity.
- Include the office contact details for any follow-ups regarding the authorization request.
- Complete the group number and NPI (National Provider Identifier) fields as required, to provide additional identification for verification.
- Enter the mailing address, including city, state, and ZIP code, to ensure proper communication.
- Fill in the primary phone number for the patient or the prescriber for any necessary contact.
- If applicable, include the specialty or facility name, along with its contact number to direct inquiries appropriately.
- Specify the state license ID of the prescriber to further validate their authority in making the request.
- Indicate whether the request is expedited or urgent, depending on the patient's needs.
- Clearly state the drug name and its strength to specify which medication is being requested.
- Provide directions or SIG (Signa) for how the medication is to be administered.
- Attach any relevant medical history or information that may support the approval of the authorization request.
- Answer the diagnostic question by selecting the applicable diagnosis and provide the relevant ICD-9 code(s).
- Indicate if the patient has failed at least one prior systemic therapy with a 'Yes' or 'No' choice.
- Provide any additional comments or information that might assist in the decision-making process.
- Obtain the prescriber’s signature in the designated area to validate the request.
- Finally, review the entire form for completeness, and save changes to store your information. You can also download, print, or share the completed form as needed.
Complete your Prior Authorization Form - Swhp online today to expedite your medication approval process.
The healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patient's insurance provider. As mentioned in the “How does prior authorization work?” section above, this will then often prompt a time-consuming back and forth between the provider and payer.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


