Loading
Get Presbyterian Prior Authorization
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Presbyterian Prior Authorization online
Filling out the Presbyterian Prior Authorization form online can be a straightforward process when you know the necessary steps. This guide will provide clear instructions to help you effectively complete the form and submit it for approval.
Follow the steps to complete the Presbyterian Prior Authorization form online.
- Press the ‘Get Form’ button to access the Presbyterian Prior Authorization form and open it in your digital editor.
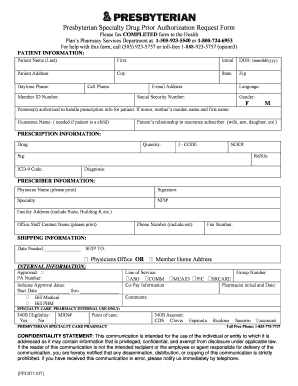
- In the Patient Information section, enter the patient's last name, first name, and initial. Provide the date of birth in the format mm/dd/yyyy, along with the patient’s address, city, state, and zip code.
- Fill in the patient's daytime and cell phone numbers, member ID number, and email address. Indicate the preferred language and provide the patient’s Social Security number and gender.
- If applicable, list individuals authorized to handle prescription information for the patient. This is especially important if the patient is a minor; include the mother’s maiden name and first name.
- Specify the patient’s relationship to the insurance subscriber, such as spouse, child, or relative.
- In the Prescription Information section, input the medication name, required quantity, J-Code, NDC number, dosage instructions (sig), refills needed, ICD-9 code, and diagnosis.
- Proceed to the Prescriber Information section and enter the physician's name, signature, specialty, NPI number, facility address (including suite/building number), office staff contact name, phone number with extension, and fax number.
- For Shipping Information, indicate the date needed and choose whether to ship to the physician’s office or the member's home address.
- Fill out the Internal Information section, including the approval status, PA number, approval dates, billing details, group number, and co-pay information.
- Review and finalize any additional comments in the designated section. Ensure all information is accurate.
- Once completed, remember to save changes to the document, and you may then download, print, or share the form as necessary.
Complete your Presbyterian Prior Authorization form online today for a streamlined process.
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


