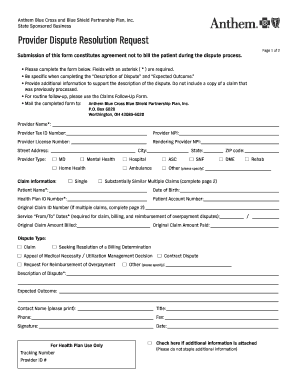
Get Anthem Provider Dispute Resolution Request
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Anthem Provider Dispute Resolution Request online
Filing a dispute resolution request can be a critical process for resolving issues related to claims. This guide provides step-by-step instructions on how to complete the Anthem Provider Dispute Resolution Request online, ensuring that you provide all necessary information effectively.
Follow the steps to complete your dispute resolution request online
- Click the ‘Get Form’ button to access the Anthem Provider Dispute Resolution Request and open it in the designated editor.
- Begin by filling in the provider's information, including the provider name, tax ID number, NPI, and license number. Ensure accuracy as this information is essential for processing your request.
- Provide the street address, city, state, and ZIP code for the provider. Select the appropriate provider type from the options available.
- Fill out the claim information section. Specify whether it pertains to a single claim, hospital, ASC, DME, or other categories. For multiple claims, remember to complete page two of the form.
- Enter the patient’s name, date of birth, health plan ID number, and patient account number. Ensure that the details match the client's records.
- In the dispute section, indicate the original claim ID number and the service dates. This date information is crucial for billing and reimbursement disputes.
- Detail the original claim amounts billed and paid. This financial information helps clarify the dispute.
- Select the type of dispute you are filing. Options include claim disputes, appeals of medical necessity, reimbursement requests, or contract disputes.
- In the 'Description of Dispute' field, provide a detailed account of the issue. Be specific and clear to facilitate the review process. Also, outline the expected outcome of your dispute.
- Complete the contact name, title, phone number, and fax number fields for communication purposes. This will ensure you can be reached regarding the dispute.
- Finally, sign and date the form to validate your submission. Once completed, you can save the changes, download, print, or share the form accordingly.
Take the first step in resolving your claims disputes by completing the Anthem Provider Dispute Resolution Request online today.
You typically have a limited timeframe to appeal a claim with Anthem, usually within 180 days of receiving your denial notice. It is crucial to act quickly and prepare your Anthem Provider Dispute Resolution Request as soon as possible. Failing to meet this deadline may result in losing your right to dispute the claim. Stay proactive to ensure your appeal is considered.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


