Loading
Get Prior Authorization Request Form - Unity Health Insurance
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Request Form - Unity Health Insurance online
Filling out the Prior Authorization Request Form for Unity Health Insurance can be a straightforward process if you follow the right steps. This guide provides you with comprehensive instructions to ensure that you complete the form accurately and efficiently.
Follow the steps to complete the Prior Authorization Request Form online
- Press the ‘Get Form’ button to access the form and open it for editing.
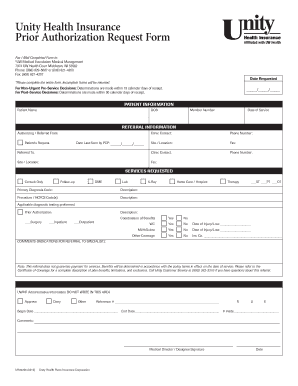
- Begin by entering the date requested in the relevant field at the top of the form.
- Provide the patient information, including the patient's name, date of birth, member number, and expected date of service.
- Fill in the referral information section. Include details for both the authorizing/referred from and referred to clinics, including contact names, phone numbers, locations, and fax numbers.
- Indicate the patient’s request by noting the date last seen by the primary care provider.
- In the services requested section, select the type of service by checking the relevant box (e.g., consult only, follow-up, DME, etc.). Provide the primary diagnosis code and a description.
- For procedures or HCPCS codes, enter the relevant information and descriptions for any requested home care, hospice, or therapy services.
- Complete the coordination of benefits section by checking 'yes' or 'no' for applicable coverages (e.g., WC, MVA/Subro), and fill in the date of injury or loss if applicable.
- Add any additional comments or indications for referral to the specialist as necessary.
- Once all sections are filled out, review the form carefully to ensure all fields are complete, as incomplete forms will be returned.
- After confirming your information is correct, you can save the changes, download, print, or share the form as needed.
Start filling out your Prior Authorization Request Form online today for a smooth submission process.
The following information is generally required for all prior authorization letters. The demographic information of the patient (name, date of birth, insurance ID number and more) Provider information (both referring and servicing provider) ... Requested service/procedure along with specific CPT/HCPCS codes.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


