Get Wellcare Dme Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Wellcare Dme Authorization Form online
The Wellcare Dme Authorization Form is essential for obtaining necessary medical equipment and services. This guide provides clear, step-by-step instructions for completing the form online, ensuring you can navigate the process efficiently.
Follow the steps to complete the Wellcare Dme Authorization Form online.
- Press the ‘Get Form’ button to access the Wellcare Dme Authorization Form and open it in your preferred editor.
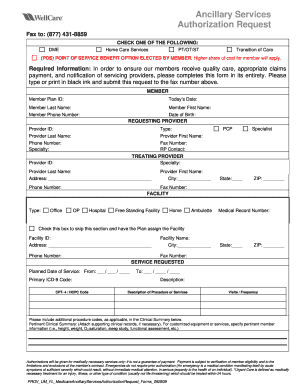
- Begin filling out the 'Member' section. Enter the Member Plan ID, today's date, member's last name, first name, phone number, and date of birth.
- Next, navigate to the 'Requesting Provider' section. Here, provide the primary care provider's ID, type, last name, first name, phone number, specialty, and fax number.
- In the 'Treating Provider' section, fill in the treating provider's ID, specialty, last name, first name, address (including city, state, and ZIP code), phone number, and fax number.
- Proceed to the 'Facility' section, where you may specify the facility type (Office, OP, Hospital, Free Standing Facility, Home, Ambulette). If necessary, you can check the box to skip this section and allow the plan to assign a facility.
- In the 'Service Requested' section, indicate the planned date of service, primary ICD-9 code, CPT-4 / HCPC code, and the description of the procedure or services required.
- Fill in the visits and frequency for the requested service. If applicable, attach a pertinent clinical summary that provides additional procedures codes and necessary member information.
- Once all information is entered, review the form for accuracy. Finally, save your changes. You can choose to download, print, or share the form as needed.
Complete your Wellcare Dme Authorization Form online today for a smoother process!
The prior authorization process involves several steps to ensure the medical necessity of a treatment. Initially, your healthcare provider evaluates your condition and decides if prior authorization is needed. They then submit the Wellcare Dme Authorization Form to the insurance provider for review. Once reviewed, the provider will inform you about the approval or denial, allowing you to make informed decisions about your care.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


