Loading
Get Prior Authorization Criteria Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Criteria Form online
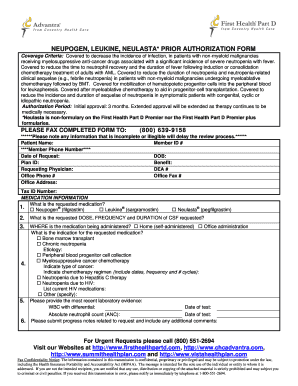
Completing the Prior Authorization Criteria Form online can be an essential step in securing necessary medical treatments. This guide will walk you through the process step-by-step, ensuring all required information is provided.
Follow the steps to complete the form accurately.
- Click ‘Get Form’ button to obtain the form and open it in your preferred editor.
- Enter the patient's personal details in the designated fields, including their name, member ID, phone number, date of birth, and plan ID.
- Fill out the benefit section and provide the details for the requesting physician: their name, DEA number, office phone number, office fax number, office address, and tax ID number.
- In the medication information section, mark the requested medication by checking the relevant box for ®, ®, or ®.
- Specify the requested dose, frequency, and duration of the medication by filling in the corresponding fields.
- Indicate where the medication will be administered by selecting either home or office administration.
- Provide the indication for the requested medication by checking the appropriate box and filling in any additional details regarding type of cancer and chemotherapy regimen, including dates and frequency.
- Complete the section requiring the most recent laboratory evidence including WBC with differential and absolute neutrophil count, along with the dates of tests.
- Submit progress notes related to the request, including any additional comments that may support the authorization.
- If requesting an exception to the plan's utilization management requirements, fill out the relevant section with clear details outlining the patient's situation.
- Finally, review all entered information for accuracy, then save changes, download, print, or share the form as necessary.
Start filling out your forms online today to ensure timely processing.
To complete the prior authorization process, you generally need to submit the Prior Authorization Criteria Form along with supporting documents. These documents may include medical records, test results, and a letter of medical necessity. Check with your insurance provider for any additional requirements. Using our platform can help you gather and submit all necessary documents efficiently.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


