Get Silverscript Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Silverscript Prior Authorization Form online
Filling out the Silverscript Prior Authorization Form online can be straightforward when you understand the process. This guide provides clear, step-by-step instructions to help you complete the form accurately and efficiently.
Follow the steps to complete the Silverscript Prior Authorization Form.
- Click 'Get Form' button to obtain the form and open it for editing.
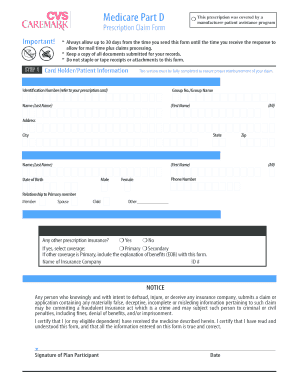
- In the Card Holder/Patient Information section, fill out all required details to ensure proper reimbursement. This includes the identification number, group number, name, address, state, city, and zip code.
- Provide patient information. Use a separate claim form for each individual. Enter the patient's name, date of birth, relationship to the primary member, and phone number.
- Indicate whether there is any other prescription insurance coverage. If so, provide information about the insurance company and include an explanation of benefits if the other coverage is primary.
- In the submission requirements section, gather and attach all necessary original pharmacy receipts. Note that cash register receipts are only accepted for diabetic supplies.
- Ensure that each pharmacy receipt includes the patient's name, date of fill, total charge, prescription number, medicine NDC number, metric quantity, days supply, and pharmacy name and address or pharmacy NABP number.
- Follow the mailing instructions provided on the form based on the RXBIN number on your CVS Caremark Prescription ID card, ensuring that you mail to the correct P.O. Box.
- Before submitting, double-check that all information is complete and accurate. After reviewing, you can save changes, download the form, print it for records, or share it as needed.
Complete your Silverscript Prior Authorization Form online today and streamline your prescription claim process.
No, individuals cannot submit their own prior authorization requests directly to SilverScript. It's a requirement that your healthcare provider completes the SilverScript Prior Authorization Form and submits it on your behalf. This ensures that all necessary medical information is accurately presented. If you have questions or need guidance, the US Legal Forms platform can assist you in finding the right forms and resources.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


