Get 866 250 2005 Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the 866 250 2005 Prior Authorization Form online
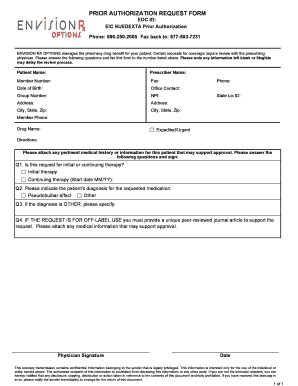
Filling out the 866 250 2005 Prior Authorization Form online is a straightforward process that ensures your request for medication coverage is properly submitted. This guide will walk you through each section of the form, providing clear instructions to help you complete it accurately.
Follow the steps to complete the Prior Authorization Form successfully.
- Click 'Get Form' button to obtain the form and open it in the editor.
- Enter the patient's name in the designated field to identify the individual for whom the authorization is being requested.
- Input the prescriber’s name in the section provided to ensure the request is linked to the appropriate healthcare provider.
- Fill in the member number, which is essential for identifying the patient’s coverage details.
- Include the patient's date of birth to confirm their identity and age.
- Provide office contact details to facilitate communication regarding the authorization request.
- Enter the group number associated with the patient’s insurance plan.
- Fill in the prescriber's National Provider Identifier (NPI) to validate their ability to prescribe medication.
- Complete the address fields for both the patient and prescriber to ensure accurate correspondence.
- Document the phone number for contact purposes, making it easier for the reviewer to reach you if necessary.
- Tick the option for expedited or urgent request if applicable.
- Enter the name of the drug requested, along with specific directions for its use.
- Attach any pertinent medical history or supporting information that justifies the authorization request.
- Answer the question regarding whether this is for initial or continuing therapy by selecting the appropriate box.
- Indicate the patient's diagnosis for the requested medication to provide context for the request.
- If the diagnosis is other, specify it in the provided section.
- If the request is for off-label use, attach a peer-reviewed journal article that supports the request.
- Have the prescriber sign and date the form to validate the request before submission.
- Review all filled sections for completeness and accuracy, ensuring no information is left blank or illegible.
- Upon confirmation of completeness, save changes, download, print, or share the completed form as needed.
Complete your authorization requests online today for a seamless process.
To submit prior authorization for medication to Medicare, start by completing the 866 250 2005 Prior Authorization Form, which outlines the medication details and reason for the request. Your healthcare provider will usually assist you in this process, as they need to submit the form on your behalf. Make sure all necessary documentation is included to support your request. This thoroughness can lead to a timely response from Medicare.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


