Get This Form Is To Be Used To Obtain Prior Authorization For Greater Then ...
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the This Form Is To Be Used To Obtain Prior Authorization For Greater Than Three Obstetric Ultrasounds online
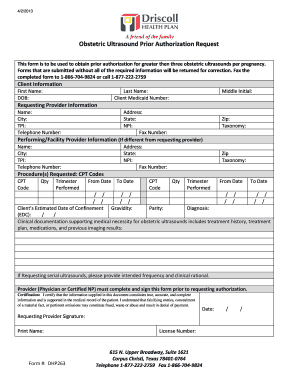
This guide provides step-by-step instructions on how to effectively fill out the form used to obtain prior authorization for more than three obstetric ultrasounds per pregnancy. Following these directions will help ensure that you submit a complete and accurate request.
Follow the steps to complete your prior authorization request effectively
- Click the ‘Get Form’ button to access the prior authorization form and open it for completion.
- Begin by filling in the client information section. Provide the first name, date of birth, last name, and client Medicaid number as required. Ensure that this information is accurate to avoid delays.
- Next, complete the requesting provider information section. You will need to include your name, address, city, state, tax identification number (TPI), telephone number, national provider identifier (NPI), and fax number.
- If the performing or facility provider is different from the requesting provider, fill out their details in the appropriate section including name, address, city, state, TPI, NPI, telephone number, and fax number.
- In the procedure(s) requested section, list the CPT codes for the obstetric ultrasounds being requested. Make sure to specify the quantity for each code, the trimester when they will be performed, and the date range if applicable.
- Provide the client’s estimated date of confinement, gravidity, and parity information in the designated fields.
- Attach the clinical documentation supporting the medical necessity for the obstetric ultrasounds. This documentation should include treatment history, treatment plan, medications, and previous imaging results.
- If requesting serial ultrasounds, clearly state the intended frequency and provide clinical rationale for the request.
- Ensure that the provider, whether a physician or certified nurse practitioner, completes and signs the form to validate the request.
- Finally, review all entries for accuracy before submitting the form. You can then save changes, download, print, or share the completed form as needed. Fax the completed form to 1-866-704-9824 or call 1-877-222-2759 with any questions.
Complete your prior authorization request online today to ensure timely processing.
The point of prior authorization is to verify that the medical services or medications proposed are medically necessary before they are provided to the patient. This process helps manage costs for both the patient and insurance provider while ensuring that the recommended care meets established medical standards. This form is to be used to obtain prior authorization for greater than the treatments that may require additional scrutiny. Thus, it helps protect patients from unexpected expenses and ensures they receive appropriate care.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


