Loading
Get Network Health Unemployment Prior Auth Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Network Health Unemployment Prior Auth Form online
Filling out the Network Health Unemployment Prior Auth Form online can be straightforward with the right guidance. This comprehensive guide will walk you through each section of the form, ensuring that you provide all necessary information accurately.
Follow the steps to complete the Network Health Unemployment Prior Auth Form online.
- Click ‘Get Form’ button to obtain the form and open it for filling.
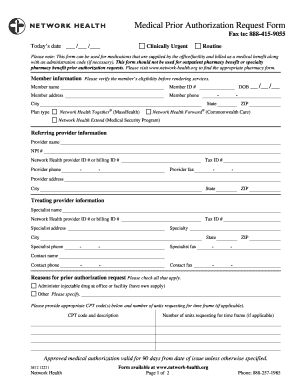
- Begin by providing today's date in the designated field at the top of the form. Ensure you select whether the request is clinically urgent or routine.
- In the member information section, enter the member's name, member ID number, address, phone number, city, date of birth, state, plan type, and ZIP code. Verify the member’s eligibility before submitting the form.
- Complete the referring provider information section. Include the provider's name, NPI number, Network Health provider ID or billing ID, phone number, tax ID, fax number, and address including city, state, and ZIP code.
- Fill in the treating provider information with the specialist’s name, Network Health provider ID or billing ID, tax ID, address, specialty, phone number, and fax number.
- In the reasons for prior authorization request section, check all applicable boxes, including administering injectable drugs at an office or facility. Include appropriate CPT codes and the number of units requested.
- Indicate the primary and secondary diagnosis in the diagnosis section by entering the corresponding ICD-9 codes.
- In the requested services section, specify the number of visits requested and the first date of services. If there are other specific requests, describe them accordingly.
- Fill out the drug information section with the name and strength of the requested drug, NDC number, dose, frequency of administration, J-code, and the number of J-code units.
- In the additional clinical information field, document any other medications the member has tried or failed. You may include a copy of a chart or progress note if necessary.
- Once all sections of the form are completed, you can save your changes, download the form, print it, or share it as needed.
Take the next step in managing your unemployment prior authorization by completing the form online today.
Yes, UnitedHealthcare does require prior authorization for many treatments and services. This process allows them to confirm that the provided care meets established clinical guidelines. It’s best to consult the Network Health Unemployment Prior Auth Form to understand what requires authorization under your specific plan.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


