Get Precertification Aetna
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Precertification Aetna online
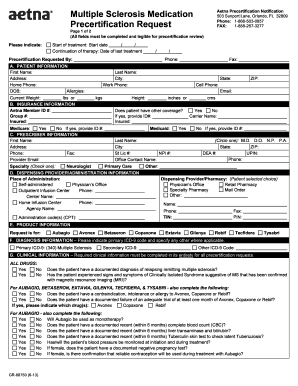
Completing the Precertification Aetna form is an essential step for obtaining authorization for multiple sclerosis medication. This guide will walk you through each section of the form, ensuring you provide all necessary information accurately and efficiently.
Follow the steps to complete your precertification request.
- Click ‘Get Form’ button to access the Precertification Aetna form and open it in the editor.
- Indicate your treatment start date and the date of the last treatment. Ensure these dates are clear and accurately filled in.
- Complete the Patient Information section with the patient's first name, last name, address, and contact information, including phone numbers and email address.
- Fill in the Insurance Information section. Include the Aetna Member ID number, group number, and whether the patient has additional coverage.
- Complete the Prescriber Information, entering the prescriber's name, contact details, and professional identifiers such as NPI number.
- In the Dispensing Provider/Administration Information section, choose the place of administration and provide relevant contact details.
- Select the product requested from the list of medications for multiple sclerosis treatment.
- Indicate the primary ICD-9 diagnosis code and any secondary codes if applicable.
- Complete the Clinical Information section by answering all questions thoroughly to ensure a smooth review process.
- Finally, complete the Acknowledgment section by providing your signature and the date to validate the request before submitting.
- Review the completed form for accuracy, and then save any changes. You can download, print, or share the form as needed.
Begin your online precertification process today to ensure timely access to necessary medications.
The purpose of precertification is to ensure that patients receive medically necessary treatments while managing healthcare costs. By requiring prior approval for certain services, Aetna aims to prevent unnecessary procedures and optimize patient care. This process is an essential step in the Precertification Aetna protocol, aligning treatment plans with coverage policies. It ultimately protects both patients and providers from unexpected financial burdens.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


