Get Anthem Prior Authorization Form Pdf
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Anthem Prior Authorization Form Pdf online
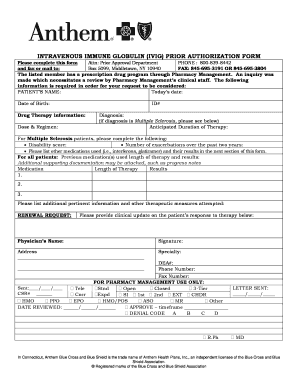
The Anthem Prior Authorization Form is a crucial document required for individuals seeking coverage approval for intravenous immune globulin therapy. This guide provides a clear and comprehensive approach to completing the form online, ensuring users can easily navigate each section.
Follow the steps to fill out the Anthem Prior Authorization Form online.
- Click ‘Get Form’ button to obtain the form and open it in your editing tool.
- Begin by entering the patient’s name in the designated field. Ensure that the spelling is accurate as this will be used for identification.
- Fill in today’s date and the patient’s date of birth in the corresponding fields. This information helps in maintaining patient records.
- Enter the patient’s ID number in the appropriate field, which is crucial for verifying the patient's account.
- Provide detailed drug therapy information, including the dose and regimen prescribed. This is essential for the clinical review process.
- Specify the patient's diagnosis. If the diagnosis is Multiple Sclerosis, additional fields for disability score and number of exacerbations over the past two years will need to be completed.
- Indicate the anticipated duration of therapy. This helps in assessing the long-term management of the patient's health.
- For those diagnosed with Multiple Sclerosis, list any other medications used along with their results in the next section.
- For all patients, provide details of previous medications, the length of therapy, and results in the specified format.
- You may include any additional pertinent information or other therapeutic measures attempted in the provided space.
- If this is a renewal request, please provide a clinical update on the patient’s response to the ongoing therapy.
- Fill in the physician’s name, signature, address, and specialty. The physician’s DEA number, phone number, and fax number are also required.
- Review all fields for accuracy and completeness to ensure a smooth approval process.
- Once completed, you can save changes, download, print, or share the form as needed.
Complete your forms accurately and submit them online for a smoother authorization process.
Generally, you can expect to hear back about your prior authorization within a few business days after submitting your request. However, the exact timing can vary based on the complexity of the case and the specific guidelines set forth by Anthem. To avoid surprises, use the Anthem Prior Authorization Form Pdf and follow up with Anthem for updates. Staying informed can help you manage your healthcare planning more effectively.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


