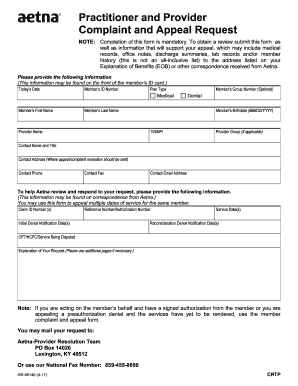
Get Aetna Practitioner And Provider Complaint And Appeal Request
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Aetna Practitioner And Provider Complaint And Appeal Request online
Filling out the Aetna Practitioner And Provider Complaint And Appeal Request form is essential for ensuring your concerns are addressed efficiently. This guide provides clear, step-by-step instructions on how to complete the form online, enabling you to submit your complaint or appeal with ease.
Follow the steps to fill out the form accurately and effectively.
- Click ‘Get Form’ button to obtain the form and open it for editing.
- Enter today’s date at the top of the form to indicate when you are submitting the request.
- Provide the member’s ID number, which can be located on the front of the member’s ID card.
- Select the plan type, which may be medical or dental, as applicable to the member.
- Fill in the member’s first and last name as shown on their ID card.
- State the provider's name associated with the complaint or appeal.
- If applicable, include the member’s group number, which is optional.
- Record the member’s birthdate in the format MM/DD/YYYY.
- Enter the provider’s TIN (Tax Identification Number) or NPI (National Provider Identifier) as required.
- If part of a provider group, include the provider group name.
- Fill in the contact person’s name and title to whom Aetna should address the response.
- Provide the contact address where the appeal or complaint resolution should be sent.
- Include the contact phone number for any further communication Aetna may need to initiate.
- Add the contact fax number if applicable.
- Enter the contact email address for electronic correspondence.
- List claim ID numbers, reference numbers, or authorization numbers related to the request if available.
- Indicate the initial denial notification dates and service dates pertinent to the complaint or appeal.
- Provide reconsideration denial notification dates and details of the service being disputed using CPT or HCPC codes.
- Formulate a clear and detailed explanation of your request. Utilize additional pages as necessary to fully express your concerns.
- Once completed, save changes to the document, and choose to download, print, or share the form as necessary.
Ensure timely processing of your complaint or appeal by completing the form online today.
Timeframes for reconsiderations and appeals Dispute levelDoctor / provider submission timelineAetna response timeframeAppealsWithin 60 calendar days of the previous decision.*Within 60 business days of receiving the request. If additional information is needed, within 60 calendar days of receiving that information.1 more row
Fill Aetna Practitioner And Provider Complaint And Appeal Request
To obtain a review, you'll need to submit this form. Make sure to include any information that will support your appeal. Aetna's 180-day dispute filing standard will apply. The exceptions below apply to requests regarding members covered under fully insured plans only. How do I file a dispute or appeal, or check on my request? Online: Use the Availity provider website to file your request and check status. File a non-Medicare complaint online. If you have a non-Medicare plan, just click the button below to file your complaint. State regulations or your provider contract may allow more time. Within 180 calendar days of the initial claim decision.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


