Loading
Get Cdphp Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Cdphp Prior Authorization Form online
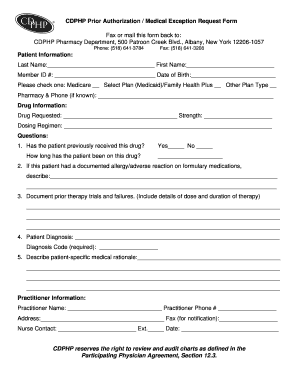
Navigating the Cdphp Prior Authorization Form can be essential for obtaining necessary medications. This guide provides step-by-step instructions to help users fill out the form online accurately and confidently.
Follow the steps to successfully complete the form.
- Click the ‘Get Form’ button to access the Cdphp Prior Authorization Form and open it for editing.
- Begin with the patient information section. Fill in the last name, first name, member ID number, and date of birth. Specify the patient's plan type by checking the appropriate box for Medicare, Select Plan (Medicaid)/Family Health Plus, or Other Plan Type. If known, include the pharmacy and its phone number.
- In the drug information section, enter the drug being requested, its strength, and specify the dosing regimen.
- Answer the initial questions regarding the patient's history with the drug. Indicate whether the patient has previously received this drug and for how long. Include additional details for allergies or adverse reactions related to formulary medications.
- Document any prior therapy trials and failures. Be sure to include information on the dose and duration of each therapy.
- Provide the patient's diagnosis and include the diagnosis code, which is required for processing.
- Describe the patient-specific medical rationale supporting the authorization request. This section is crucial for justifying the need for the requested medication.
- Complete the practitioner information by entering the name, phone number, address, and fax number for notification. Include the contact details for any nurse involved in the request.
- Once all sections are filled out accurately, save your changes. You can then download, print, or share the completed form as needed.
Encourage others to complete their forms online for a seamless submission process.
Performing a prior authorization involves gathering the necessary details about your treatment or medication and submitting the Cdphp Prior Authorization Form. It’s key to work closely with your healthcare provider, as they have experience with this process. They can effectively communicate with the insurance company to facilitate approval. Keeping your provider informed and engaged will enhance your chances of a successful authorization.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


