Loading
Get Bcbsfl Prior Authorization Form Tecidera
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Bcbsfl Prior Authorization Form Tecidera online
This guide provides clear instructions for filling out the Bcbsfl Prior Authorization Form Tecidera online. By following these steps, users can ensure a smooth submission process and provide all necessary information accurately.
Follow the steps to complete the form effectively.
- Click ‘Get Form’ button to obtain the form and open it in the online editor.
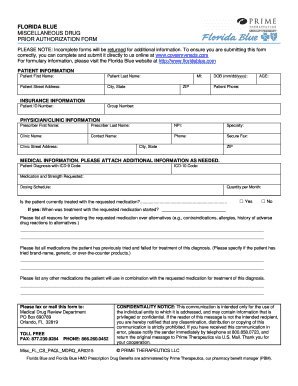
- Enter the patient information in the respective fields. This includes the patient's first name, last name, street address, city, state, and ZIP code, along with their date of birth and age. Also, include the patient’s primary phone number.
- Fill in the insurance information by entering the patient ID number and group number in the provided sections.
- Complete the physician/clinic information by providing the prescriber's first name, last name, National Provider Identifier (NPI), specialty, clinic name, and contact information. It is important to include the clinic's address as well.
- In the medical information section, specify the patient's diagnosis using the ICD-9 or ICD-10 codes. List the requested medication along with its strength and dosing schedule. Indicate the quantity per month needed.
- Answer whether the patient is currently being treated with the requested medication by selecting 'Yes' or 'No'. If 'Yes', state when treatment started.
- Provide reasons for choosing the requested medication over alternatives, detailing any contraindications, allergies, or adverse drug reactions.
- List all medications the patient has previously tried for this diagnosis, specifying if they are brand-name, generic, or over-the-counter products.
- Identify any medications that will be used in combination with the requested medication for this diagnosis.
- Complete the prescription section, indicating whether the patient will use Prime Therapeutics Specialty Pharmacy. Provide medication details, including name, form, strength, directions, frequency, and quantity.
- Make sure to include the prescriber’s signature to validate the prescription before submission.
- After completing the form, review all entries for accuracy, save any changes, and download or print the form if needed to retain a copy.
- Submit the form as instructed, either via fax to the Medical Drug Review Department or as specified online.
Complete your document submission online for a seamless process.
To obtain a prior authorization for medication with Blue Cross Blue Shield of Texas, start by contacting your healthcare provider. They will assist you in completing and submitting the necessary Bcbsfl Prior Authorization Form Tecidera. Additionally, verify that all required information is included to facilitate a smooth approval process. Clear communication with your provider can make a difference.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


