Get Optumrx & Prior Authorization Request Form 2015
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the OPTUMRx & Prior Authorization Request Form online
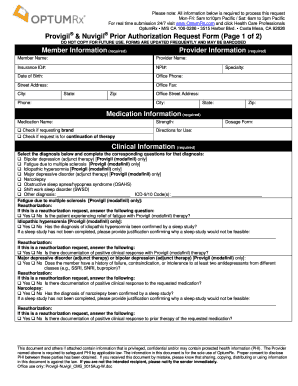
Filling out the OPTUMRx & Prior Authorization Request Form online can be a straightforward process with the right guidance. This document ensures that all necessary information is collected to efficiently process requests for medication prior authorization.
Follow the steps to complete your request form successfully.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin with the member information section. Fill in the member's name, insurance ID number, date of birth, and contact details including phone and address.
- Next, complete the provider information. Enter the provider's name, NPI number, office phone, and address details.
- In the medication information section, specify the medication name, strength, directions for use, and whether you are requesting a brand or if this is a continuation of therapy.
- Proceed to the clinical information section. Choose the diagnosis from the provided list and answer any related questions that follow. Be mindful to provide exact details and documentation if reauthorization is requested.
- If applicable, fill out the responses for each diagnosis, confirming whether the diagnosis was validated by a sleep study and providing justification if not.
- For quantity limit requests, clearly outline the requested amount per day and the reason for exceeding any plan limitations.
- Add any additional comments or important information regarding the patient's condition or previous medication trials in the comments section to assist in the review process.
- Finally, review all provided information for accuracy and completeness. Once confirmed, save your changes, download, print, or share the completed form as necessary.
Start your request now by completing the OPTUMRx & Prior Authorization Request Form online.
Get form
The time it takes for Optum Rx to process prior authorizations can vary depending on several factors, including the specific medication requested. Generally, you can expect a response within a few business days. However, in some cases, additional information may be required, which can extend the wait time. Staying connected with the provider can help you monitor progress and resolve any issues that arise.
Get This Form Now!
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


