Get Humana Pain Management Prior Authorization Request Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Humana Pain Management Prior Authorization Request Form online
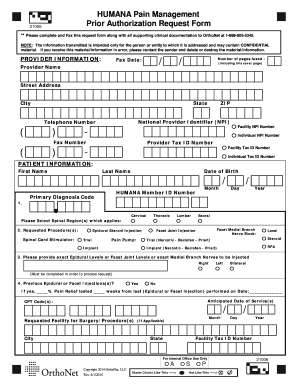
Filling out the Humana Pain Management Prior Authorization Request Form online is a straightforward process designed to help providers efficiently submit requests for patient procedures. This guide will walk you through each step of the form to ensure you provide all necessary information accurately.
Follow the steps to complete the Humana Pain Management Prior Authorization Request Form.
- Press the ‘Get Form’ button to access and open the request form.
- Begin by entering the provider information. Fill in the provider name, fax date, number of pages faxed, street address, city, state, national provider identifier (NPI), telephone number, and both facility and individual tax ID numbers.
- Next, provide the patient information. Enter the patient's first name, last name, date of birth, Humana member ID number, and the primary diagnosis code.
- Select the spinal region(s) that apply by indicating cervical, thoracic, lumbar, or sacral.
- In this section, list the requested procedure(s). Indicate whether you are requesting a spinal cord stimulator, epidural steroid injection, pain pump, facet medial branch nerve block, or facet joint injection, among others.
- Provide the exact epidural levels, facet joint levels, or medial branch nerves to be injected. Specify right, left, or bilateral as necessary.
- Indicate if previous epidural or facet injections were administered. If yes, specify the percentage of pain relief and the duration it lasted, including the date the last injection was performed.
- Lastly, fill in the anticipated date of service(s), CPT code(s), requested facility for surgery or procedure(s), and the facility's tax ID number.
- Review all entries for accuracy, save your changes, and decide whether to download, print, or share the completed form.
Complete your Humana Pain Management Prior Authorization Request Form online today to ensure timely processing of patient care.
To ask for pre-authorization, you should first consult with your healthcare provider, who will guide you through the necessary steps. They will complete the required forms, such as the Humana Pain Management Prior Authorization Request Form, and submit them to your insurance company on your behalf. Open communication with your provider helps ensure that you understand the process and receive timely guidance.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


