Loading
Get Ky Aetna Pharmacy Prior Authorization Request Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the KY Aetna Pharmacy Prior Authorization Request Form online
Filling out the KY Aetna Pharmacy Prior Authorization Request Form online can seem daunting, but with clear guidance, you can navigate it successfully. This guide provides detailed, step-by-step instructions tailored to your needs to ensure all required information is accurately submitted.
Follow the steps to complete the form online.
- Click the ‘Get Form’ button to access the form and open it in your preferred editor.
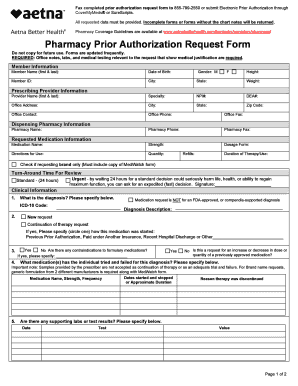
- Enter the member information, including the member's full name, date of birth, member ID, city, state, weight, and the provider's details such as their name, specialty, NPI number, DEA number, office address, contact information, and pharmacy details.
- Input the requested medication information, including the medication name, strength, dosage form, directions for use, and quantity, as well as the gender and height of the member.
- Indicate the duration of therapy, refills needed, and whether you are requesting brand only. If applicable, ensure you include a copy of the MedWatch form.
- Provide clinical information, starting with the diagnosis and corresponding ICD-10 code, followed by any contraindications to formulary medications and previous medication trials.
- Complete all additional fields for supporting labs or test results, and include any critical extra information pertinent to the review, including safety concerns and the reasons for requesting a specific medication.
- Sign and date the form, confirming the accuracy of the provided information. Remember to check if additional information is needed based on specific medications.
- Once all sections are fully completed, you can save the changes, download, print, or share the form as needed.
Complete the KY Aetna Pharmacy Prior Authorization Request Form online today to ensure timely processing.
The phone number for Aetna Better Health of Kentucky provider services is 1-866-474-8275. This dedicated line helps you get any assistance you may need, including questions about the KY Aetna Pharmacy Prior Authorization Request Form. Don’t hesitate to call if you require support during your authorization process.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


