Get Cigna Great West Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Cigna Great West Prior Authorization Form online
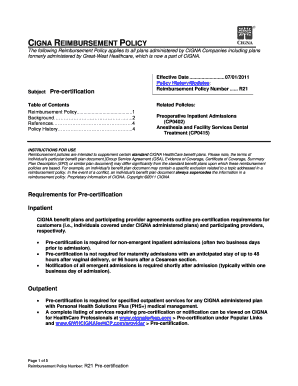
Completing the Cigna Great West Prior Authorization Form online can streamline the approval process for necessary medical services. This guide provides a detailed, step-by-step approach to ensure that you accurately fill out the form, helping you to avoid any delays in care.
Follow the steps to successfully complete the form online.
- Press the ‘Get Form’ button to acquire the authorization form and open it for editing.
- Begin by entering the participant's name and identification number in the designated fields. This information is crucial as it identifies the individual who is seeking prior authorization.
- Provide the participant's date of birth. Ensure this matches the records held by Cigna to avoid any discrepancies.
- Include the diagnosis using the appropriate ICD-9-CM code. This code is essential for Cigna to understand the medical condition that requires treatment.
- List the requesting or referring healthcare professional's details. This helps in establishing accountability for the service being requested.
- Enter the servicing healthcare professional's information, including the vendor or facility name. This ensures that Cigna can easily reach out for any necessary verification.
- Detail any pertinent medical history related to the condition. Justification for the requested service must be clearly articulated to aid in the review process.
- Specify the anticipated length of stay if the request is for inpatient services. This helps Cigna assess the medical necessity for the planned treatment.
- Complete the date of request field accurately. An incorrect date can lead to processing delays.
- If applicable, mention any additional insurance coverage to provide a complete picture of the participant's healthcare resources.
- Indicate the place of service and the level of care requested, whether inpatient or outpatient.
- Finally, describe the procedure, service, or item to be pre-certified, accompanied by the appropriate CPT-4 or HCPCS code, as this is vital for accurate processing.
- After filling out all required fields, review the form for accuracy. You can then save the changes, download the form, print it, or share it for further processing.
Complete your Cigna Great West Prior Authorization Form online to ensure efficient processing of your medical services.
A prior authorization request form is a document that healthcare providers use to obtain approval for specific treatments before they are delivered. This process ensures that the proposed services are medically necessary and covered by the insurance plan. By utilizing the Cigna Great West Prior Authorization Form, healthcare providers can streamline this process and enhance patient care.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


