Get Premera Member Submitted Claim Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Premera Member Submitted Claim Form online
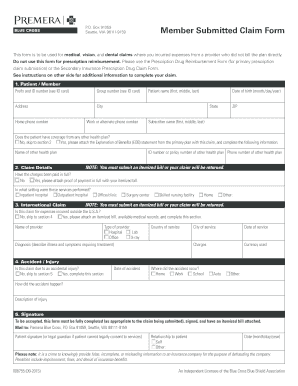
Completing the Premera Member Submitted Claim Form online is an essential process for users who need to claim reimbursement for medical, vision, and dental expenses incurred from providers who do not bill directly. This guide aims to provide clear and comprehensive instructions to help you navigate each section of the form effectively.
Follow the steps to complete your claim form accurately.
- Press the ‘Get Form’ button to obtain the claim form and open it in your preferred online editor.
- Begin by filling in the patient/member section, which includes the prefix, ID number, group number, address, city, state, ZIP code, home phone number, and work or alternate phone number. Ensure that you have your ID card ready to locate this information.
- Enter the patient’s full name (first, middle, last) and date of birth (month/day/year). If the patient has coverage from another health plan, indicate ‘Yes’ and attach the Explanation of Benefits (EOB) statement along with the name of the other health plan.
- In the claim details section, provide the ID number or policy number of the other health plan, the phone number for that plan, and whether the charges have been paid in full. If not, include proof of payment alongside the itemized bill.
- Specify the setting where the services were performed, selecting from options such as inpatient hospital, outpatient hospital, office/clinic, or others. Remember, you must submit an itemized bill; otherwise, your claim will be returned.
- If the claim pertains to services incurred outside the U.S.A., mark ‘Yes’ and complete the section with the provider's name, type of provider, country of service, diagnosis, city of service, date of service, charges, and the currency used.
- In the accident/injury section, answer if the claim is due to an accidental injury. If ‘Yes,’ provide the date of the accident, location, and a description of how the accident occurred.
- Finally, review all entries for completeness. Ensure that the form is fully completed where necessary, signed by the patient or a legal guardian, and that the itemized bill is attached.
- Once completed, save your changes, download a copy for your records, print it for mailing, or share it with relevant parties as needed.
Ensure that you complete your claim form online accurately to expedite processing.
A claim form, such as the Premera Member Submitted Claim Form, is a document that policyholders submit to request reimbursement or a benefit from their insurer. It serves as an official record of the services rendered, expenses incurred, or incidents leading to the claim. Accurate completion of this form is crucial for a smooth claims process.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


