Get Prior Authorization Form - Priority Health 2020-2025
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form - Priority Health online
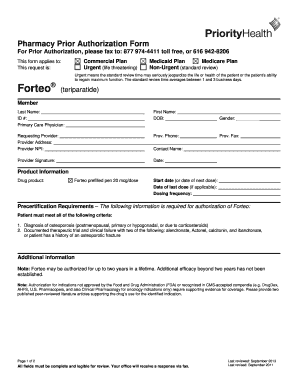
Filling out the Prior Authorization Form for Priority Health is a critical step in ensuring that necessary medications are approved for coverage. This guide provides clear, step-by-step instructions to help users navigate the process of completing the form accurately and efficiently online.
Follow the steps to complete the Prior Authorization Form successfully.
- Click ‘Get Form’ button to obtain the form and open it for editing.
- Begin by filling in the 'Member' section, which includes the last name, first name, ID number, date of birth, and gender of the member.
- Provide details of the 'Primary Care Physician,' including their name and contact information.
- In the 'Requesting Provider' section, enter the provider's name, address, NPI number, phone number, and fax number.
- Ensure the provider's signature and date are provided to confirm the request.
- Fill in the 'Product Information' section with the drug product details, including the product name, start date, date of last dose, and dosing frequency.
- Address the 'Precertification Requirements' by listing the diagnosis of osteoporosis, and documenting any therapeutic trials and clinical failures with specified medications.
- If applicable, provide additional information regarding the patient's condition and any necessary supporting evidence, especially if none of the precertification criteria are met.
- Review all fields to make sure they are complete and legible.
- Once all sections are filled out correctly, users can save changes, download, print, or share the completed form as needed.
Complete your Prior Authorization Form online for a smoother approval process.
Certain services, such as expensive medical procedures, specialized treatment, and some prescription medications, often require prior authorization. The specific requirements can vary by insurance plan, so checking the guidelines of the patient's health insurance, including those from Priority Health, is essential. To navigate these requirements confidently, the Prior Authorization Form - Priority Health can provide clear instructions.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


