Authorization Letter For Medicine Purchase Without Bill
Description
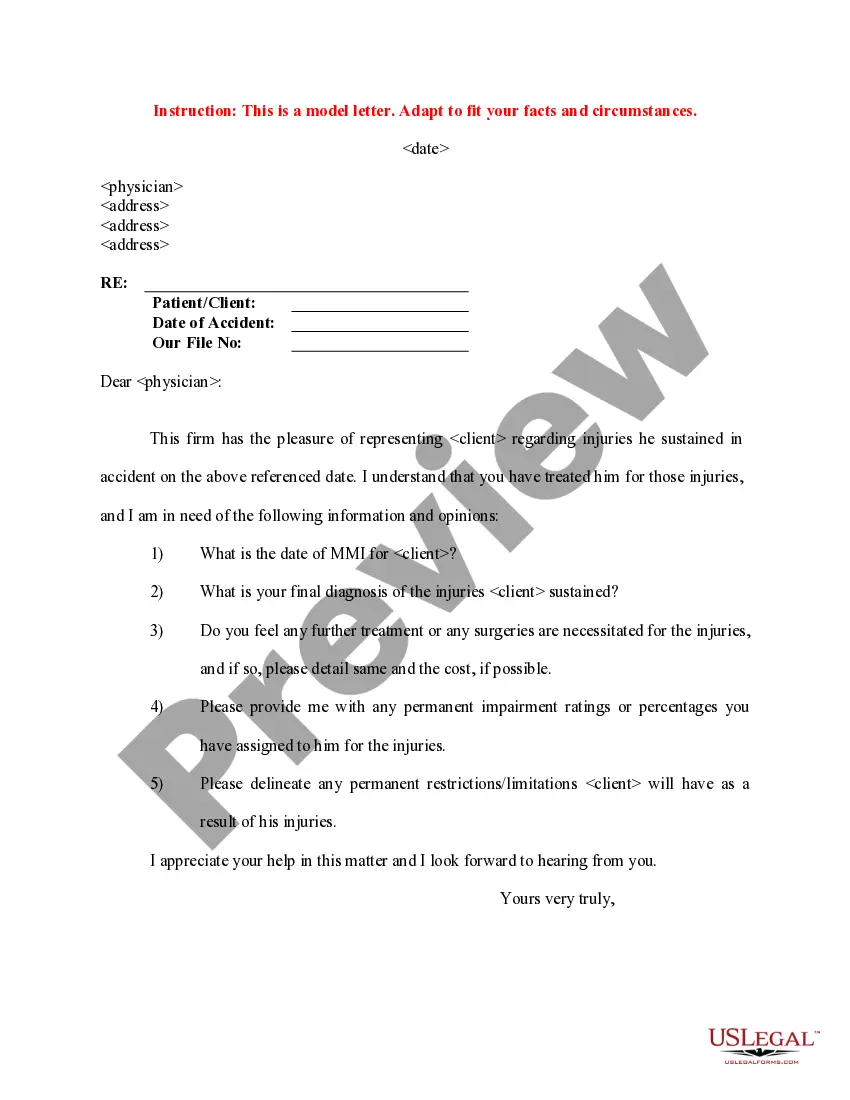
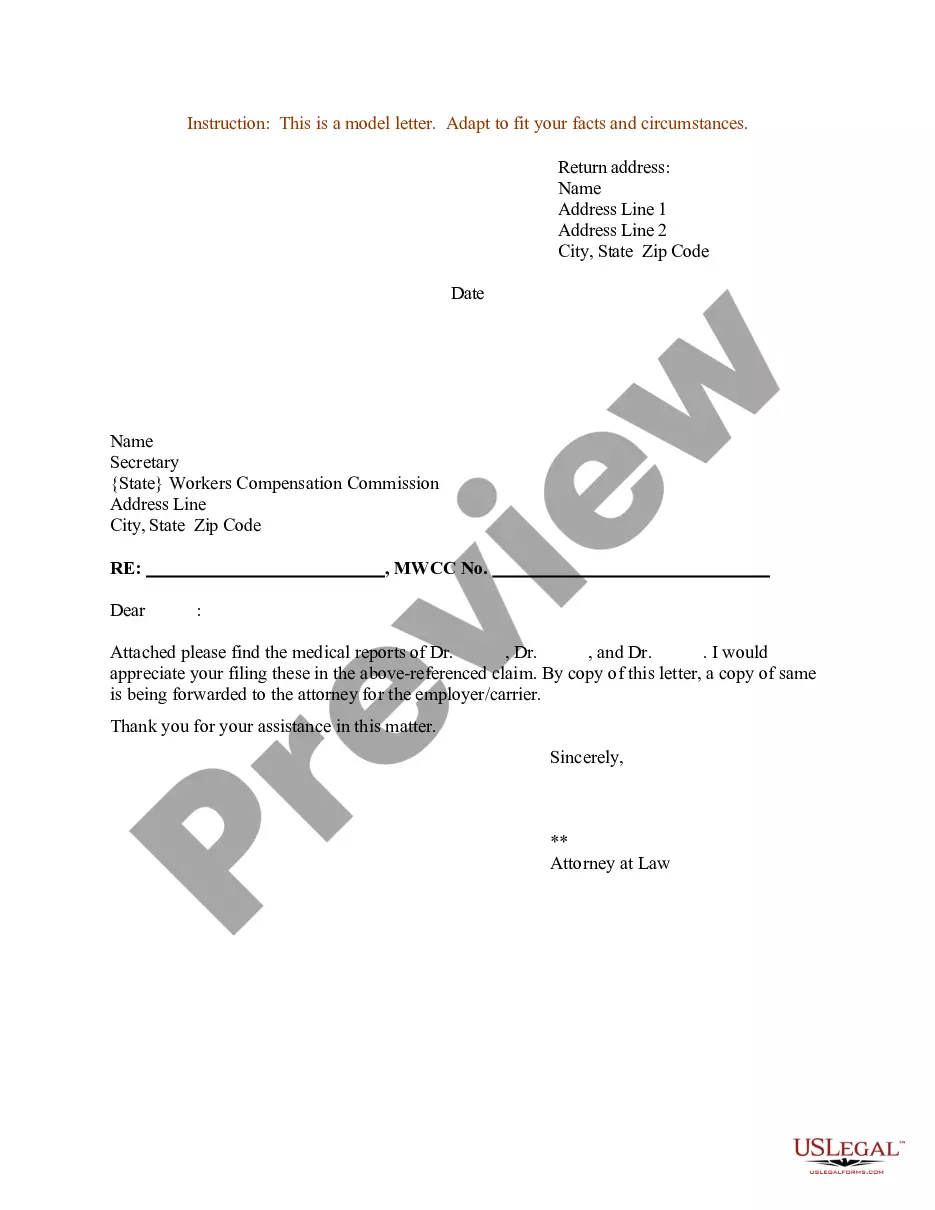
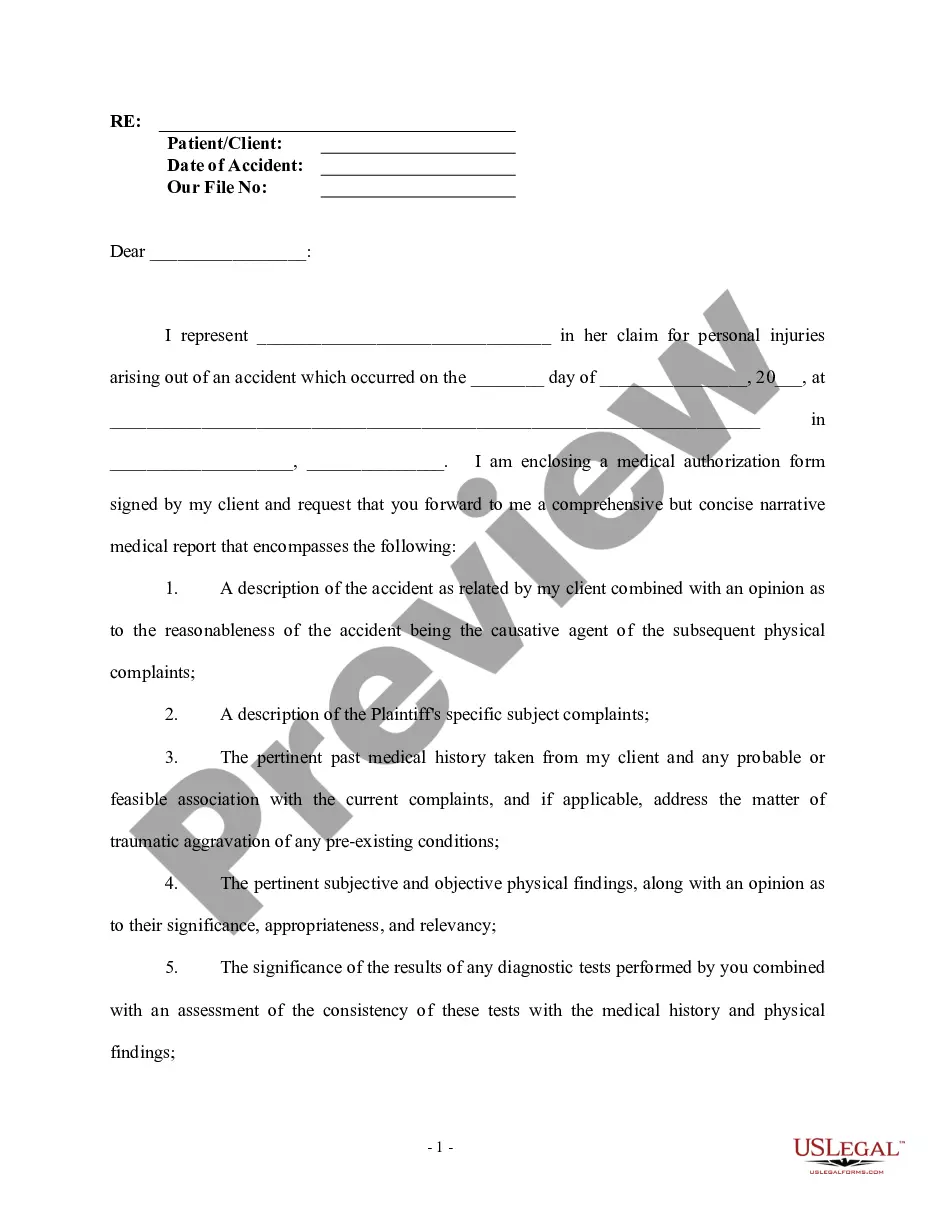
How to fill out Sample Letter For Medical Authorization For Client Medical History?
The Authorization Letter For Medicine Acquisition Without Invoice that you observe on this site is a versatile legal template formulated by expert attorneys in accordance with federal and state statutes.
For over 25 years, US Legal Forms has supplied individuals, businesses, and lawyers with over 85,000 validated, state-specific documents for any personal and professional occasion. It’s the fastest, simplest, and most dependable method to secure the paperwork you require, as the service assures bank-level data security and anti-malware safeguards.
Subscribe to US Legal Forms to have validated legal templates for all of life's situations at your convenience.
- Search for the document you require and examine it.
- Browse the file you looked for and preview it or review the form description to ensure it meets your needs. If it does not, use the search feature to find the correct one. Click Buy Now when you have located the template you need.
- Select and Log In.
- Choose the pricing plan that fits you and establish an account. Use PayPal or a credit card for a swift transaction. If you already possess an account, Log In and check your subscription to continue.
- Acquire the editable template.
- Choose the format you prefer for your Authorization Letter For Medicine Purchase Without Bill (PDF, Word, RTF) and download the document to your device.
- Complete and sign the forms.
- Print the template to fill it out manually. Alternatively, use an online multi-functional PDF editor to quickly and accurately complete and sign your form with an eSignature.
- Download your documents again.
- Use the same document again whenever required. Access the My documents tab in your profile to redownload any previously acquired forms.
Form popularity
FAQ
What Happens When Pre-Authorization Is Not Done? If pre-authorization in medical billing is not obtained from the insurance company, a claim could be delayed, denied, or only partially approved with reduced reimbursement rates. In many cases, the medical organization might absorb all or part of the cost.
Prior authorization?sometimes called precertification or prior approval?is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Dear <Medical Director Name and/or Medical Review/Appeals>: I am writing to request authorization for <Product Name> for my patient, <Patient Name>. I have prescribed <Product Name> because this patient has been diagnosed with <diagnosis>, and I believe that therapy with <Product Name> is appropriate for this patient.
However, there are some instances ? such as when a patient is out of network ? that it may be appropriate to charge for a prior auth. In this scenario, the physician would not have a contract with the patient's health plan and could theoretically charge for the preauthorization.
Foremost Task: Ensure the CPT code is Correct Best Practices for Prior Authorization: ... Keep Necessary Information Ready : ... Follow recommended treatment guidelines: ... Meet all Payer Criteria: ... Get Preauthorization for Mundane Procedures: ... Monitor Insurance Carrier Websites Regularly: ... Update Contracts with Insurance Companies: