Sample Physician Letter Of Incompetence For A Doctor
Description
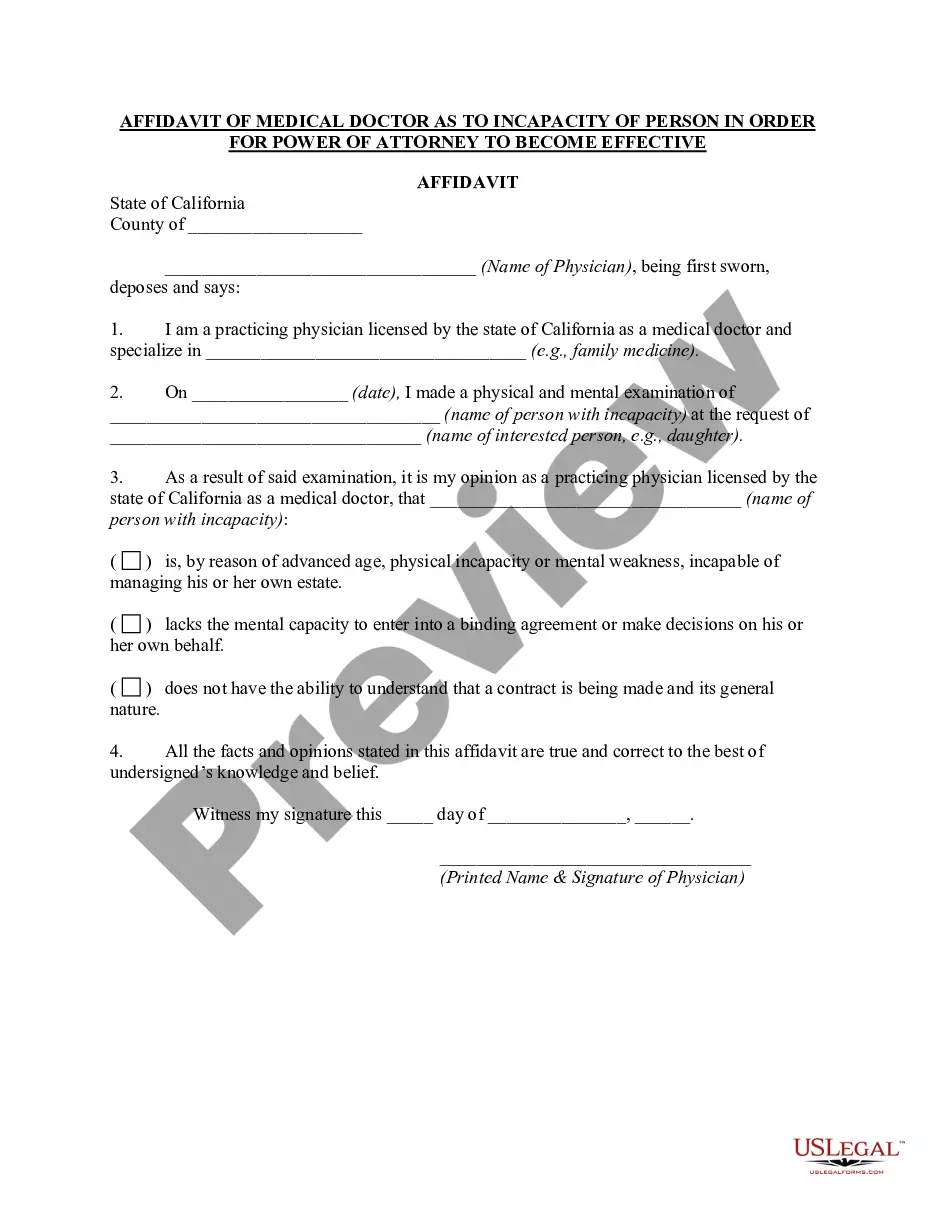
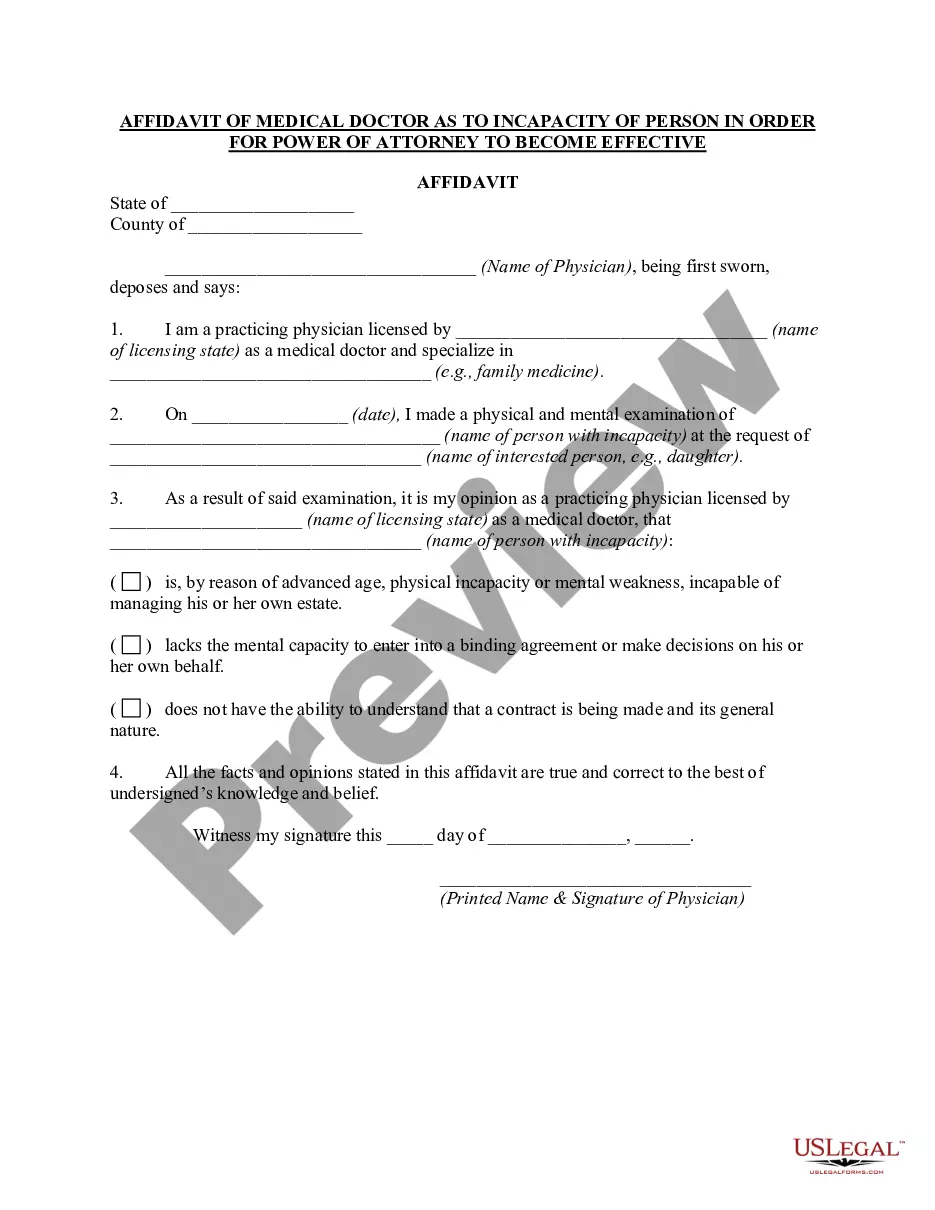
How to fill out California Affidavit Of Medical Doctor As To Incapacity Of Person In Order For Power Of Attorney To Become Effective?
Managing legal documents can be perplexing, even for the most experienced professionals.
If you're searching for a Sample Physician Letter of Incompetence for a Doctor but lack the opportunity to find the suitable and current version, the experience can be quite overwhelming.
Access a valuable repository of articles, guides, handbooks, and materials relevant to your circumstances and requirements.
Save time and effort in your search for necessary documents and use US Legal Forms’ advanced search and Preview feature to find the Sample Physician Letter of Incompetence for a Doctor and download it.
Take advantage of the US Legal Forms web catalog, supported by 25 years of experience and trustworthiness. Transform your document management into a seamless and user-friendly experience today.
- If you have a subscription, Log In to your US Legal Forms account, search for the form, and download it.
- Check your My documents tab to view previously downloaded documents and manage your folders as needed.
- If this is your first time using US Legal Forms, create an account for unlimited access to all the resources in the library.
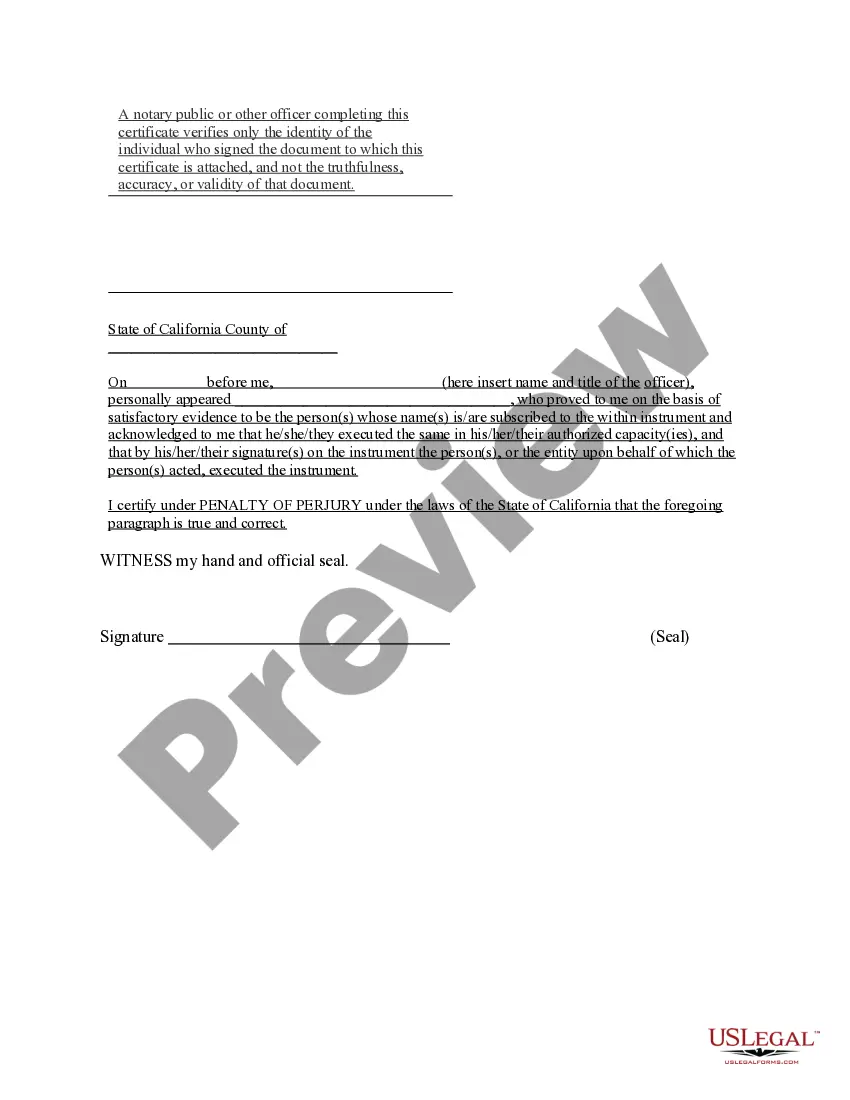
- After downloading the required form, verify it by previewing and checking its description.
- Ensure the sample is accepted in your state or county.
- Select Buy Now when you’re prepared.
- Choose a subscription plan.
- Select the desired file format, and then Download, complete, eSign, print, and deliver your documents.
- Access state- or county-specific legal and business documents.
- US Legal Forms addresses all your requirements, from personal to commercial paperwork, all in one location.
- Utilize cutting-edge tools to complete and manage your Sample Physician Letter of Incompetence for a Doctor.
Form popularity
FAQ
A letter of medical necessity (LOMN) is a document from your licensed healthcare provider that recommends a particular treatment, product, or equipment for medical purposes. The letter often includes relevant patient history, medical needs, and the duration of the treatment.
Dear: [Contact Name/Medical Director], I am writing on behalf of my patient, [Patient First and Last Name] to document the medical necessity for treatment with [DRUG NAME]. This letter provides information about the patient's medical history, diagnosis and a summary of the treatment plan.
The [PATIENT NAME] has a diagnosis of [DIAGNOSIS] and needs treatment with [INSERT PRODUCT], and that [INSERT PRODUCT] is medically necessary for [him/her] as prescribed. On behalf of the patient, I am requesting approval for use and subsequent payment for the [TREATMENT].
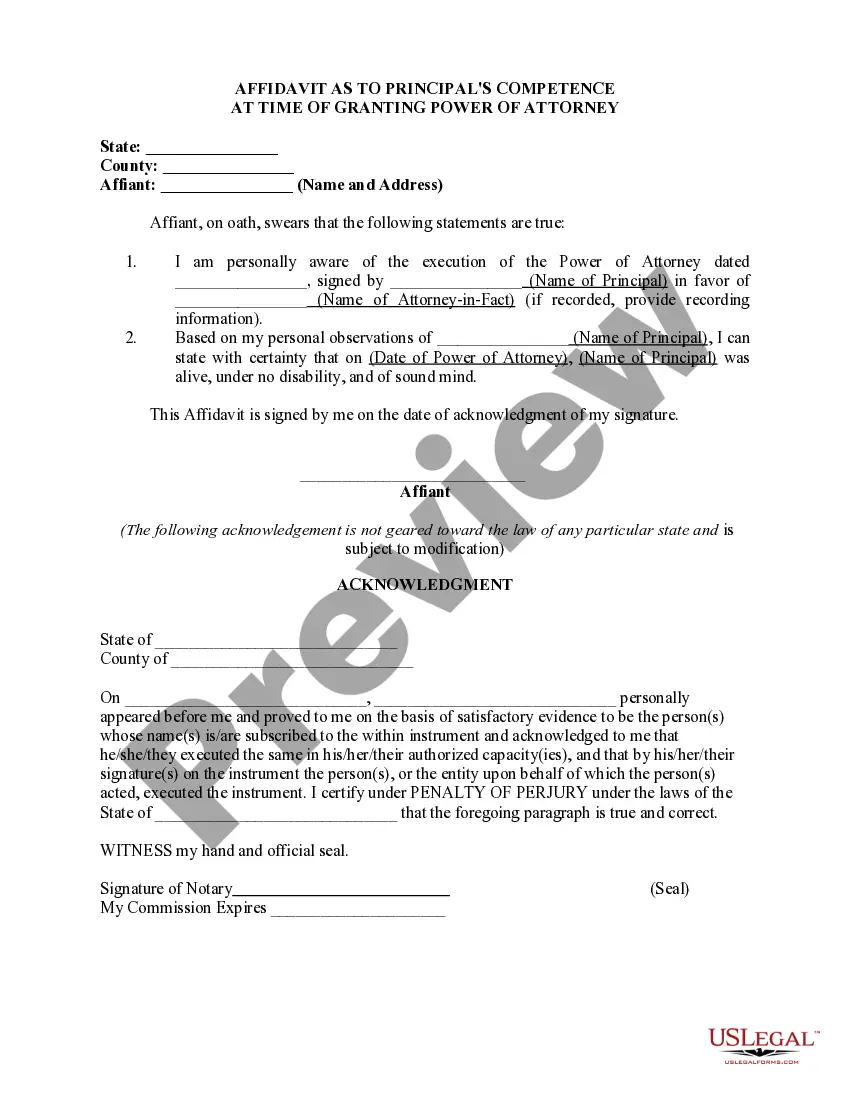
When it comes to a letter of capacity, letter of incapacitation, or medical incapacity letter, these are all different ways to say the same thing. A letter of capacity and a letter of competency are both drawn up and signed by a licensed physician to be presented in court to establish guardianship or conservatorship.
Sample Format Letter of Medical Necessity Dear [Insert Contact Name]: [Insert Patient Name] has been under my care for [Insert Diagnosis] [Insert ICD-10-CM Code] since [Insert Date]. Treatment of [Insert Patient Name] with [medication] is medically appropriate and necessary and should be covered and reimbursed.